- Record: found
- Abstract: found
- Article: found
Electrocardiographic methods for diagnosis and risk stratification in the Brugada syndrome
Read this article at
Abstract
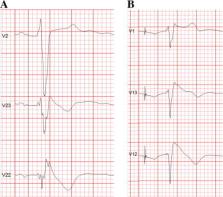
The Brugada syndrome (BrS) is a malignant, genetically-determined, arrhythmic syndrome manifesting as syncope or sudden cardiac death (SCD) in individuals with structurally normal hearts. The diagnosis of the BrS is mainly based on the presence of a spontaneous or Na + channel blocker induced characteristic, electrocardiographic (ECG) pattern (type 1 or coved Brugada ECG pattern) typically seen in leads V1 and V2 recorded from the 4th to 2nd intercostal (i.c.) spaces. This pattern needs to be distinguished from similar ECG changes due to other causes (Brugada ECG phenocopies). This review focuses mainly on the ECG-based methods for diagnosis and arrhythmia risk assessment in the BrS. Presently, the main unresolved clinical problem is the identification of those patients at high risk of SCD who need implantable cardioverter-defibrillator (ICD), which is the only therapy with proven efficacy. Current guidelines recommend ICD implantation only in patients with spontaneous type 1 ECG pattern, and either history of aborted cardiac arrest or documented sustained VT (class I), or syncope of arrhythmic origin (class IIa) because they are at high risk of recurrent arrhythmic events (up to 10% or more annually for those with aborted cardiac arrest). The majority of BrS patients are asymptomatic when diagnosed and considered to have low risk (around 0.5% annually) and therefore not indicated for ICD. The majority of SCD victims in the BrS, however, had no symptoms prior to the fatal event and therefore were not protected with an ICD. While some ECG markers such as QRS fragmentation, infero-lateral early repolarisation, and abnormal late potentials on signal-averaged ECG are known to be linked to increased arrhythmic risk, they are not sufficiently sensitive or specific. Potential novel ECG-based strategies for risk stratification are discussed based on computerised methods for depolarisation and repolarisation analysis, a composite approach targeting several major components of ventricular arrhythmogenesis, and the collection of large digital ECG databases in genotyped BrS patients and their relatives.
Related collections
Most cited references89
- Record: found
- Abstract: found
- Article: not found
Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report.
- Record: found
- Abstract: found
- Article: not found
Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry.
- Record: found
- Abstract: found
- Article: not found