- Record: found
- Abstract: found
- Article: found
Metabolic syndrome and insulin resistance in obese adolescents Translated title: Síndrome metabólico y resistencia a la insulina en adolescentes obesos
Read this article at
Abstract
Objective:
To verify the prevalence of metabolic syndrome and insulin resistance in obese adolescents and its relationship with different body composition indicators.
Methods:
A cross-sectional study comprising 79 adolescents aged ten to 18 years old. The assessed body composition indicators were: body mass index (BMI), body fat percentage, abdominal circumference, and subcutaneous fat. The metabolic syndrome was diagnosed according to the criteria proposed by Cook et al. The insulin resistance was determined by the Homeostasis Model Assessment for Insulin Resistance (HOMA-IR) index for values above 3.16. The analysis of ROC curves was used to assess the BMI and the abdominal circumference, aiming to identify the subjects with metabolic syndrome and insulin resistance. The cutoff point corresponded to the percentage above the reference value used to diagnose obesity.
Results:
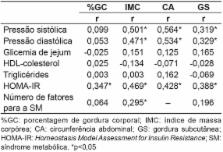
The metabolic syndrome was diagnosed in 45.5% of the patients and insulin resistance, in 29.1%. Insulin resistance showed association with HDL-cholesterol ( p=0.032) and with metabolic syndrome ( p=0.006). All body composition indicators were correlated with insulin resistance ( p<0.01). In relation to the cutoff point evaluation, the values of 23.5 and 36.3% above the BMI reference point allowed the identification of insulin resistance and metabolic syndrome. The best cutoff point for abdominal circumference to identify insulin resistance was 40%.
Translated abstract
Verificar la prevalencia del síndrome metabólico y de la resistencia a la insulina en adolescentes obesos y su relación con distintos indicadores de composición corporal.
Estudio transversal con 79 adolescentes de 10 a 18 años. Los indicadores de composición corporal fueron: índice de masa corporal (IMC), porcentaje de grasa corporal, circunferencia abdominal y grasa subcutánea. El síndrome metabólico fue diagnosticado conforme a los criterios de Cook et al. La resistencia a la insulina fue determinada por el índice de Homeostasis Model Assessment for Insulin Resistence (HOMA-IR) para valores superiores a 3,16. Se utilizó el análisis de curvas ROC para evaluar el IMC y la circunferencia abdominal, identificándose los individuos con resistencia a la insulina y síndrome metabólico. El punto de corte correspondió al porcentaje superior al valor de referencia para el diagnóstico de obesidad.
El síndrome metabólico fue diagnosticado en 45,5% de los pacientes y la resistencia a la insulina, en 29,1%. La resistencia a la insulina presentó asociación con el HDL-colesterol ( p=0,032) y con el síndrome metabólico ( p=0,006). Todos los indicadores de composición corporal evaluados presentaron correlación con la resistencia a la insulina ( p<0,01). En la evaluación de los puntos de corte, los valores de 23,5 y 36,3% por encima del valor de referencia del IMC permitieron identificar la resistencia a la insulina y el síndrome metabólico. El mejor punto de corte de la circunferencia abdominal para identificar la resistencia a la insulina fue de 40%.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935.
- Record: found
- Abstract: found
- Article: not found
Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents.
- Record: found
- Abstract: found
- Article: not found