- Record: found
- Abstract: found
- Article: not found
“Prediabetes”: Are There Problems With This Label? No, We Need Heightened Awareness of This Condition!
Read this article at
Abstract
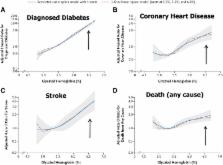
The category of “prediabetes” defined by the American Diabetes Association comprises a range of intermediate hyperglycemia based on fasting or 2-h postload glucose or on HbA 1c. Over the recent past, the “cut points” identifying this stage have changed, i.e., a lower fasting glucose level is used. On one hand, it can be argued that the change to a lower cut point identifies a group of individuals still at higher risk and provides heightened awareness for a condition associated with higher risk for cardiovascular disease. In addition, identification of individuals at this stage may represent a chance of earlier intervention in the disease. However, the argument against this definition of prediabetes is that it disguises the differences in the three subcategories and creates problems in interpreting observations on interventions and outcomes. In addition, it can be argued that the enormous numbers of people identified with the criteria far exceeds the capacity of health care systems to respond through individual care, particularly without evidence that interventions benefit any category other than impaired glucose tolerance. Thus, there does not appear to be consensus on the definition using the cut points identified. Controversy also remains as to whether there are glycemic metrics beyond HbA 1c that can be used in addition to HbA 1c to help assess risk of an individual developing diabetes complications. Given the current controversy, a Point-Counterpoint debate on this issue is provided herein. In the preceding point narrative, Dr. Yudkin provides his argument that there are significant problems with this label. In the counterpoint narrative below, Dr. Cefalu argues that the cut points are appropriate and do provide useful and important information in trying to reduce the future burden of diabetes.
—William T. Cefalu
Editor in Chief, Diabetes Care
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose.
- Record: found
- Abstract: found
- Article: not found
Normal fasting plasma glucose levels and type 2 diabetes in young men.
- Record: found
- Abstract: found
- Article: not found
