- Record: found
- Abstract: found
- Article: found
The effect of diagnostic criteria on outcome measures in preclinical and prodromal Alzheimer's disease: Implications for trial design
Read this article at
Abstract
Introduction
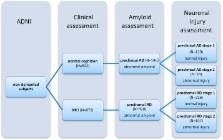
We investigated the influence of different inclusion criteria for preclinical and prodromal Alzheimer's disease (AD) on changes in biomarkers and cognitive markers and on trial sample size estimates.
Methods
We selected 522 cognitively normal subjects and 872 subjects with mild cognitive impairment from the Alzheimer's Disease Neuroimaging Initiative study. Compared inclusion criteria were (1) preclinical or prodromal AD (amyloid marker abnormal); (2) preclinical or prodromal AD stage-1 (amyloid marker abnormal, injury marker normal); and (3) preclinical or prodromal AD stage-2 (amyloid and injury markers abnormal). Outcome measures were amyloid, neuronal injury, and cognitive markers.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI.
- Record: found
- Abstract: found
- Article: found
Longitudinal change in CSF biomarkers in autosomal-dominant Alzheimer's disease.
- Record: found
- Abstract: found
- Article: not found