- Record: found
- Abstract: found
- Article: found
Oral misoprostol for preventing postpartum haemorrhage in home births in rural Bangladesh: how effective is it?
Read this article at
Abstract
Aims
Evidence exists about prevention of postpartum haemorrhage (PPH) by oral administration of misoprostol in low-income countries, but effectiveness of prevention by lay community health workers (CHW) is not sufficient. This study aimed to investigate whether a single dose (400 µg) of oral misoprostol could prevent PPH in a community home-birth setting and to assess its acceptability and feasibility among rural Bangladeshi women.
Methods
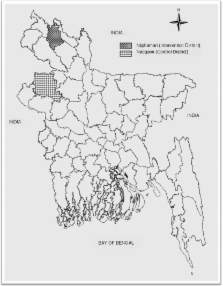
This quasi-experimental trial was conducted among 2,017 rural women who had home deliveries between November 2009 and February 2010 in two rural districts of northern Bangladesh. In the intervention district 1,009 women received 400 µg of misoprostol immediately after giving birth by the lay CHWs, and in the control district 1,008 women were followed after giving birth with no specific intervention against PPH. Primary PPH (within 24 hours) was measured by women's self-reported subjective measures of the normality of blood loss using the ‘cultural consensus model.’ Baseline data provided socio-economic, reproductive, obstetric, and bleeding disorder information.
Findings
The incidence of primary PPH was found to be lower in the intervention group (1.6%) than the control group (6.2%) ( p<0.001). Misoprostol provided 81% protection (RR: 0.19; 95% CI: 0.08–0.48) against developing primary PPH. The proportion of retained and manually removed placentae was found to be higher in the control group compared to the intervention group. Women in the control group were more likely to need an emergency referral to a higher level facility and blood transfusion than the intervention group. Unexpectedly few women experienced transient side effects of misoprostol. Eighty-seven percent of the women were willing to use the drug in future pregnancy and would recommend to other pregnant women.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Oral misoprostol in preventing postpartum haemorrhage in resource-poor communities: a randomised controlled trial.
- Record: found
- Abstract: found
- Article: not found
WHO multicentre randomised trial of misoprostol in the management of the third stage of labour.
- Record: found
- Abstract: found
- Article: not found