- Record: found
- Abstract: found
- Article: found
Case Report: Resetting the Humoral Immune Response by Targeting Plasma Cells With Daratumumab in Anti-Phospholipid Syndrome
Read this article at
Abstract
Introduction
Monoclonal antibodies (mAb) targeting plasma cells are malignant gammopathy designed and approved therapies. In recent years, these antibodies have also been increasingly introduced for non-malignant conditions such as autoimmune-mediated diseases. The Anti-Phospholipid Syndrome (APS) is an immune-mediated disorder in which autoantibodies against phospholipid associated proteins could elicit the activation of the coagulation cascade in specific situations. Therefore, the mainstream treatment for APS patients is the use of anticoagulant therapy. However, there are refractory patients who would benefit from targeting the antibodies rather than their effects. Rituximab, a B-cell depleting mAb, and intravenous immunoglobulins (IVIG) have been used in APS patients without showing a clear beneficial effect or a significant drop in anti-phospholipid antibody (aPL) levels.
Clinical case
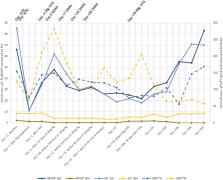
We present our first APS case treated with daratumumab, an anti-CD38 mAb, in a 21-year-old patient with APS who presented with recurrent venous thromboembolic events despite adequate anticoagulant therapy. She tested positive for lupus anticoagulant, anti-cardiolipin IgG, anti-beta-2-glycoprotein-I IgG and anti-phosphatidylserine/prothrombin IgG and IgM. She was administered one dose weekly of daratumumab for 4 weeks. The treatment showed an adequate safety profile and was well tolerated. The patient was discharged after undergoing a clinically significant improvement. After the therapy, her levels of positive aPL declined significantly and most continued to decrease during the next three months. The patient experienced a new thrombotic episode two years after the therapy associated with poor adherence to antithrombotic therapy.
Conclusions
The treatment with daratumumab showed an adequate safety profile, was well tolerated and led to a significant clinical improvement. Levels of aPL lowered on therapy and the next three months and then rose again during follow-up. Further investigation is needed to better elucidate the role and optimal timing and doses of daratumumab in treatment of refractory APS.
Related collections
Most cited references48
- Record: found
- Abstract: found
- Article: not found
International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS).
- Record: found
- Abstract: found
- Article: not found
Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer.
- Record: found
- Abstract: found
- Article: not found