- Record: found
- Abstract: found
- Article: found
Neonatal hypothermia and associated risk factors among newborns of southern Nepal
Read this article at
Abstract
Background
Neonatal hypothermia is associated with an increased mortality risk for 28 days. There are few community-based data on specific risk factors for neonatal hypothermia. Estimates of association between neonatal hypothermia in the community and risk factors are needed to guide the design of interventions to reduce exposure.
Methods
A cohort of 23,240 babies in rural southern Nepal was visited at home by field workers who measured axillary temperatures for 28 days (213,316 temperature measurements). The cumulative incidence of hypothermia (defined as < 35.0°C based on an analysis of the hypothermia-mortality risk relationship) was examined for any association with infant characteristics, care practices and parental, household, socioeconomic and demographic factors. Estimates were adjusted for age and ambient temperature.
Results
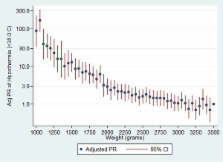
Ten percent of the babies ( n = 2342) were observed with temperatures of < 35.0°C. Adjusted prevalence ratios (Adj PR) were increased among those who weighed < 2000 g [Adj PR = 4.32 (3.73, 5.00)] or < 1500 g [Adj PR = 11.63 (8.10, 16.70)] compared to those of normal weight (> 2500 g). Risk varied inversely along the entire weight spectrum: for every 100 g decrement hypothermia risk increased by 7.4%, 13.5% and 31.3%% for babies between 3000 g and 2500 g, 2500 g and 2000 g and < 2000 g, respectively. Preterm babies (< 34 weeks), females, those who had been first breastfed after 24 h and those with hypothermic mothers were at an increased risk. In the hot season the risk disparity between smaller and larger babies increased. Hypothermia was not associated with delayed bathing, hat wearing, room warming or skin-to-skin contact: they may have been practiced reactively and thereby obscured any potential benefit.
Conclusions
In addition to season in which the babies were born, weight is an important risk factor for hypothermia. Smaller babies are at higher relative risk of hypothermia during the warm period and do not receive the protective seasonal benefit apparent among larger babies. The need for year-round thermal care, early breastfeeding and maternal thermal care should be emphasized. Further work is needed to quantify the benefits of other simple neonatal thermal care practices.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Delayed breastfeeding initiation increases risk of neonatal mortality.
- Record: found
- Abstract: found
- Article: not found
Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial.
- Record: found
- Abstract: found
- Article: not found