- Record: found
- Abstract: found
- Article: found
The role of CAT in evaluating the response to treatment of patients with AECOPD
Abstract
Background
The chronic obstructive pulmonary disease (COPD) Assessment Test (CAT) questionnaire is a short patient-completed questionnaire, which is used to assess the health status of patients with stable COPD. However, whether it is a good tool to evaluate the response to treatment in acute exacerbation of COPD (AECOPD) has been less studied.
Methods
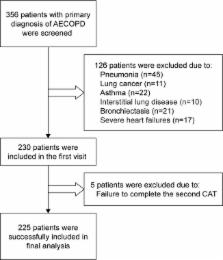
The patients were assessed at two visits, at admission and on the seventh day. Anthropometric variables were collected at admission. CAT and lung function were measured twice at the above time points. At the second visit, the health status of the patients were divided into five groups based on a 5-point Likert scale, ranging from 1 to 5, which represents “much better,” “slightly better,” “no change,” “slightly worse,” and “much worse.” Responders were those who reported “much better” or “slightly better,” and nonresponders were those who claimed “no change,” “worse,” or “much worse.”
Results
In total, 225 patients were recruited. The average CAT score at admission was 24.82±7.41, which declined to 17.41±7.35 on the seventh day. There were 81.33% responders, whose improvement in CAT score (9.37±5.24) was much higher than that of the nonresponders (−1.36±4.35). A moderate correlation was observed between the changes in CAT score and improvement in FEV 1, FEV 1%, and the length of hospital stay. There was a strong correlation between the changes in CAT score and health status. A 3.5-unit improvement in the CAT score, with highest area under the curve, was the cutoff to differentiate responders from nonresponders.
Conclusion
The evolution of CAT scores during exacerbation can provide useful information to assess the health status of patients with AECOPD. A 3.5-unit improvement in CAT score is the best cutoff to differentiate between patients who have a response or no response to treatment, which offers a convenient and easy way for clinicians to monitor the health status of patients with an AECOPD.
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Responsiveness and MCID Estimates for CAT, CCQ, and HADS in Patients With COPD Undergoing Pulmonary Rehabilitation: A Prospective Analysis.

- Record: found
- Abstract: found
- Article: found
Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ)
- Record: found
- Abstract: found
- Article: not found