- Record: found
- Abstract: found
- Article: found
“Current concepts of mechanical ventilation in neonates” – Part 1: Basics
Read this article at
Abstract
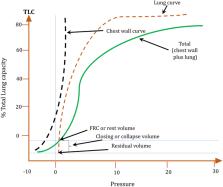
Mechanical ventilation is potentially live saving in neonatal patients with respiratory failure. The main purpose of mechanical ventilation is to ensure adequate gas exchange, including delivery of adequate oxygenation and enough ventilation for excretion of CO 2. The possibility to measure and deliver small flows and tidal volumes have allowed to develop very sophisticated modes of assisted mechanical ventilation for the most immature neonates, such as volume targeted ventilation, which is used more and more by many clinicians. Use of mechanical ventilation requires a basic understanding of respiratory physiology and pathophysiology of the disease leading to respiratory failure. Understanding pulmonary mechanics, elastic and resistive forces (compliance and resistance), and its influence on the inspiratory and expiratory time constant, and the mechanisms of gas exchange are necessary to choose the best mode of ventilation and adequate ventilator settings to minimize lung injury. Considering the pathophysiology of the disease allows a physiology-based approach and application of these concepts in daily practice for decision making regarding the use of modes and settings of mechanical ventilation, with the ultimate aim of providing adequate gas exchange and minimising lung injury.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Mechanical ventilation of the premature neonate.
- Record: found
- Abstract: found
- Article: not found