- Record: found
- Abstract: found
- Article: found
Targeting protein tyrosine phosphatase σ after myocardial infarction restores cardiac sympathetic innervation and prevents arrhythmias

Read this article at
Abstract
Millions of people suffer a myocardial infarction (MI) every year, and those who survive have increased risk of arrhythmias and sudden cardiac death. Recent clinical studies have identified sympathetic denervation as a predictor of increased arrhythmia susceptibility. Chondroitin sulfate proteoglycans present in the cardiac scar after MI prevent sympathetic reinnervation by binding the neuronal protein tyrosine phosphatase receptor σ (PTPσ). Here we show that the absence of PTPσ, or pharmacologic modulation of PTPσ by the novel intracellular sigma peptide (ISP) beginning 3 days after injury, restores sympathetic innervation to the scar and markedly reduces arrhythmia susceptibility. Using optical mapping we observe increased dispersion of action potential duration, supersensitivity to β-adrenergic receptor stimulation and Ca 2+ mishandling following MI. Sympathetic reinnervation prevents these changes and renders hearts remarkably resistant to induced arrhythmias.
Abstract
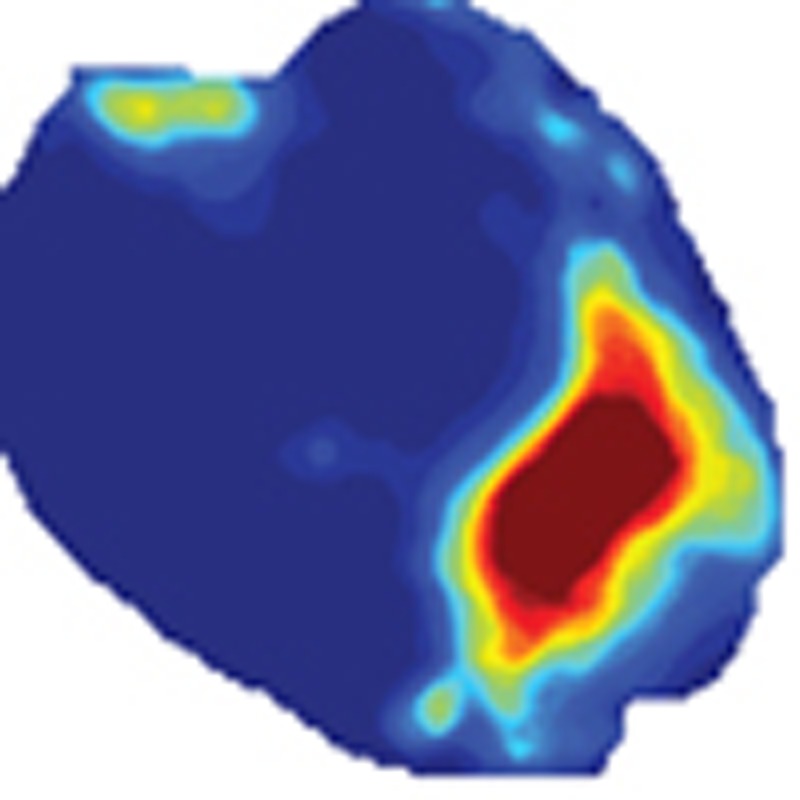 Chondroitin sulfate proteoglycans (CSP) in the myocardial scar inhibit the tissue’s
reinnervation, rendering it prone to arrhythmia. Here the authors show that blocking
the activity of the CSP receptor, protein tyrosine phosphatase receptor σ, promotes
scar reinnervation and prevents arrhythmia in mice.
Chondroitin sulfate proteoglycans (CSP) in the myocardial scar inhibit the tissue’s
reinnervation, rendering it prone to arrhythmia. Here the authors show that blocking
the activity of the CSP receptor, protein tyrosine phosphatase receptor σ, promotes
scar reinnervation and prevents arrhythmia in mice.
Related collections
Most cited references62
- Record: found
- Abstract: found
- Article: not found
Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction.
- Record: found
- Abstract: found
- Article: not found
Diabetic Hyperglycemia activates CaMKII and Arrhythmias by O linked Glycosylation
- Record: found
- Abstract: found
- Article: not found