- Record: found
- Abstract: found
- Article: not found
Noncanonical Wnt Signaling Promotes Obesity-Induced Adipose Tissue Inflammation and Metabolic Dysfunction Independent of Adipose Tissue Expansion
Read this article at
Abstract
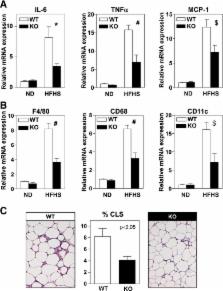
Adipose tissue dysfunction plays a pivotal role in the development of insulin resistance in obese individuals. Cell culture studies and gain-of-function mouse models suggest that canonical Wnt proteins modulate adipose tissue expansion. However, no genetic evidence supports a role for endogenous Wnt proteins in adipose tissue dysfunction, and the role of noncanonical Wnt signaling remains largely unexplored. Here we provide evidence from human, mouse, and cell culture studies showing that Wnt5a-mediated, noncanonical Wnt signaling contributes to obesity-associated metabolic dysfunction by increasing adipose tissue inflammation. Wnt5a expression is significantly upregulated in human visceral fat compared with subcutaneous fat in obese individuals. In obese mice, Wnt5a ablation ameliorates insulin resistance, in parallel with reductions in adipose tissue inflammation. Conversely, Wnt5a overexpression in myeloid cells augments adipose tissue inflammation and leads to greater impairments in glucose homeostasis. Wnt5a ablation or overexpression did not affect fat mass or adipocyte size. Mechanistically, Wnt5a promotes the expression of proinflammatory cytokines by macrophages in a Jun NH 2-terminal kinase–dependent manner, leading to defective insulin signaling in adipocytes. Exogenous interleukin-6 administration restores insulin resistance in obese Wnt5a-deficient mice, suggesting a central role for this cytokine in Wnt5a-mediated metabolic dysfunction. Taken together, these results demonstrate that noncanonical Wnt signaling contributes to obesity-induced insulin resistance independent of adipose tissue expansion.
Related collections
Most cited references52
- Record: found
- Abstract: found
- Article: not found
Developmental origin of fat: tracking obesity to its source.
- Record: found
- Abstract: found
- Article: not found
Interleukin-6-deficient mice develop mature-onset obesity.
- Record: found
- Abstract: found
- Article: not found
