- Record: found
- Abstract: found
- Article: not found
Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX™)
Read this article at
Abstract
Summary
The present study estimated the 10-year probability using the Japanese version of WHO fracture risk assessment tool (FRAX™) in order to determine fracture probabilities that correspond to intervention thresholds currently used in Japan and to resolve some issues for its use in Japan.
Introduction
The objective of the present study was to evaluate a Japanese version of the WHO fracture risk assessment (FRAX™) tool to compute 10-year probabilities of osteoporotic fracture in Japanese men and women. Since lumbar spine bone mineral density (BMD) is used preferentially as a site for assessment, and densitometers use Japanese reference data, a second aim was to investigate the suitability and impact of this practice in Japan.
Methods
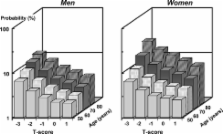
Fracture probabilities were computed from published data on the fracture and death hazards in Japan. Probabilities took account of age, sex, the presence of clinical risk factors and femoral neck BMD. Fracture probabilities were determined that were equivalent to intervention thresholds currently used in Japan. The difference between T-scores derived from international reference data and that using Japanese-specific normal ranges was estimated from published sources. The gradient of risk of BMD for fracture in Japan was compared to that for BMD at the lumbar spine in the Hiroshima cohort.
Results
The 10-year probabilities of a major osteoporosis-related fracture that corresponded to current intervention thresholds ranged from approximately 5% at the age of 50 years to more than 20% at the age of 80 years. The use of femoral neck BMD predicts fracture as well as or better than BMD tests at the lumbar spine. There were small differences in T-scores between those used for the model and those derived from a Japanese reference population.
Conclusions
The FRAX™ tool has been used to determine possible thresholds for therapeutic intervention, based on equivalence of risk with current guidelines. The approach will need to be supported by appropriate health economic analyses. Femoral neck BMD is suitable for the prediction of fracture risk among Japanese. However, when applying the FRAX™ model to Japan, T-scores and Z-scores should be converted to those derived from the international reference.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Predictive value of BMD for hip and other fractures.
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of previous fracture and subsequent fracture risk.
- Record: found
- Abstract: found
- Article: not found
