- Record: found
- Abstract: found
- Article: found
Immuno-virologic outcomes and immuno-virologic discordance among adults alive and on anti-retroviral therapy at 12 months in Nigeria
Read this article at
Abstract
Background
Predictors of immuno-virologic outcomes and discordance and their associations with clinical, demographic, socio-economic and behavioral risk factors are not well described in Nigeria since HIV viral load testing is not routinely offered in public HIV treatment programs.
Methods
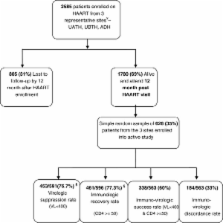
The HACART study was a multi-center observational clinic-based cohort study of 2585 adults who started HAART between April 2008 and February 2009. A total of 628 patients were randomly selected at 12 months for immuno-virologic analyses.
Results
Virologic suppression rate (<400 copies/ml) was 76.7%, immunologic recovery rate (CD4 change from baseline ≥50 cells/mm 3) was 77.4% and immuno-virologic discordance rate was 33%. In multivariate logistic regression, virologic failure was associated with age <30 years (OR 1.79; 95% CI: 1.17-2.67, p= 0. 03), anemia (Hemoglobin < 10 g/dl) (OR 1.71; 95% CI: 1.22-2.61, p= 0. 03), poor adherence (OR 3.82; 95% CI: 2.17-5.97, p= 0. 001), and post-secondary education (OR 0.60; 95% CI: 0.30-0.86, p= 0. 02). Immunologic failure was associated with male gender (OR 1.46; 95% CI: 1.04-2.45, p= 0. 04), and age <30 years (OR 1.50; 95% CI: 1.11-2.39, p= 0. 03). Virologic failure with immunologic success (VL -/CD4 +) was associated with anemia (OR 1.80; 95% CI: 1.13-2.88, p= 0. 03), poor adherence (OR 3.90; 95% CI: 1.92-8.24, p= 0. 001), and post-secondary education (OR 0.40; 95% CI: 0.22-0.68, p= 0. 005).
Conclusions
Although favorable immuno-virologic outcomes could be achieved in this large ART program, immuno-virologic discordance was observed in a third of the patients. Focusing on intensified treatment preparation and adherence, young patients, males, persons with low educational status and most importantly baseline anemia assessment and management may help address predictors of poor immuno-virologic outcomes, and improve overall HIV program impact. Viral load testing in addition to the CD4 testing should be considered to identify, characterize and address negative immuno-virologic outcomes and discordance.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa.
- Record: found
- Abstract: found
- Article: not found
Scaling up of highly active antiretroviral therapy in a rural district of Malawi: an effectiveness assessment.

- Record: found
- Abstract: found
- Article: found