- Record: found
- Abstract: found
- Article: not found
Radiological evolution of porcine neurocysticercosis after combined antiparasitic treatment with praziquantel and albendazole
Read this article at
Abstract
Background
The onset of anthelmintic treatment of neurocysticercosis (NCC) provokes an acute immune response of the host, which in human cases is associated with exacerbation of neurological symptoms. This inflammation can occur at the first days of therapy. So, changes in the brain cysts appearance may be detected by medical imaging. We evaluated radiological changes in the appearance of brain cysts (enhancement and size) on days two and five after the onset of antiparasitic treatment using naturally infected pigs as a model for human NCC.
Methods and results
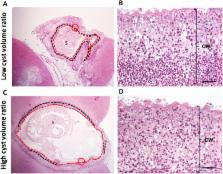
Contrast T1-weighted magnetic resonance imaging with gadolinium was performed before and after antiparasitic treatment. Eight NCC-infected pigs were treated with praziquantel plus albendazole and euthanized two (n = 4) and five (n = 4) days after treatment; another group of four infected pigs served as untreated controls. For each lesion, gadolinium enhancement intensity (GEI) and cyst volume were measured at baseline and after antiparasitic treatment. Volume and GEI quantification ratios (post/pre-treatment measures) were used to appraise the effect of treatment. Cysts from untreated pigs showed little variations between their basal and post treatment measures. At days 2 and 5 there were significant increases in GEI ratio compared with the untreated group (1.32 and 1.47 vs 1.01, p = 0.021 and p = 0.021). Cyst volume ratios were significantly lower at days 2 and 5 compared with the untreated group (0.60 and 0.22 vs 0.95, p = 0.04 and p = 0.02). Cysts with lower cyst volume ratios showed more marked post-treatment inflammation, loss of vesicular fluid and cyst wall wrinkling.
Conclusion/Significance
A significant and drastic reduction of cyst size and increased pericystic enhancement occur in the initial days after antiparasitic treatment as an effect of acute perilesional immune response. These significant changes showed that early anthelmintic efficacy (day two) can be detected using magnetic resonance imaging.
Author summary
Neurocysticercosis (NCC) is a frequent parasitic infection of the human brain and the most common cause of adult onset epilepsy in developing countries. Acute inflammatory response in NCC plays an important role in the pathogenesis of symptoms by anthelminitic therapies. The anthelmintic recommended therapy for NCC has drawbacks as the exacerbation of inflammation around degenerating cysts provokes the appearance of symptoms at the first days of treatment. Radiological changes in the appearance of cysts usually are seen after months of therapy. To evaluate if significant radiological changes (enhancement and size) occur in the first days of therapy, we used a porcine NCC model and magnetic resonance imaging (MRI) with contrast solution. The major radiological changes observed after treatment with albendazole and praziquantel were an increase in enhancement and the significant reduction in cyst size by day 2 and more evident on day 5. Cysts with greater changes also experienced exacerbated inflammation, loss of vesicular fluid and wrinkling of the cyst wall. These results show an early therapeutic effect and the possible utility of repeat MRI imaging within a few days after starting treatment. Finally, these findings contribute to our understanding of the treatment induced early exacerbation of symptoms.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Clinical symptoms, diagnosis, and treatment of neurocysticercosis.
- Record: found
- Abstract: found
- Article: not found
Diagnosis and treatment of neurocysticercosis.
- Record: found
- Abstract: found
- Article: not found
