- Record: found
- Abstract: found
- Article: found
Frailty and Its Associated Risk Factors: First Phase Analysis of Multicentre Indonesia Longitudinal Aging Study
Read this article at
Abstract
Background: National long-term care development requires updated epidemiological data related to frailty. We aimed to find the prevalence of frailty and its associated factors among Indonesian elderly.
Methods: We conducted first-phase cross-sectional analysis of Indonesia Longitudinal Aging Study (INALAS) data collected from community-dwelling outpatients aged 60 years and older without acute illness in nine geriatric service care centres. Descriptive, bivariate and multivariate analyses were conducted.
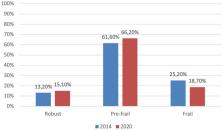
Results: Among 908 elderly in this study, 15.10% were robust, 66.20% were pre-frail, and 18.70% were frail. Functional dependence was associated with frailty among Indonesian elderly (OR 5.97, 95% CI 4.04–8.80). Being depressed and at risk for malnutrition were also associated with frailty with OR 2.54, 95% CI 1.56–4.12, and OR 2.56, 95% CI 1.68–3.90, respectively. Prior history of fall (OR 1.77, 95% CI 1.16–2.72) and hospitalization (OR 1.46, 95% CI 0.97–2.20) in the previous 12 months were associated with frailty. There is also significant association between poly pharmacy and frailty (OR 2.42, 95% CI 1.50–3.91).
Conclusion: Approximately one in five Indonesian community-dwelling elderly was frail. Frailty is associated with functional dependence, being at risk for malnutrition or being malnourished, depression, history of fall, history of hospitalization, and poly pharmacy. There may be bidirectional relationships between the risk factors and frailty. The development of long-term care in Indonesia should be considered, without forcing the elderly who need it.
Related collections
Most cited references33

- Record: found
- Abstract: found
- Article: found
What is polypharmacy? A systematic review of definitions
- Record: found
- Abstract: found
- Article: not found
Frailty consensus: a call to action.
- Record: found
- Abstract: found
- Article: not found