- Record: found
- Abstract: found
- Article: found
Postoperative morbidity of complete mesocolic excision and central vascular ligation in right colectomy: a retrospective comparative cohort study
Read this article at
Abstract
Background
To investigate morbidity and mortality following complete mesocolic excision (CME) and central vascular ligation (CVL) in patients undergoing right colectomy.
Methods
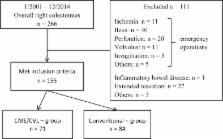
Data from consecutive patients undergoing elective right colectomy at a university-affiliated referral centre were retrospectively analysed. Patients who underwent conventional right-sided colonic cancer surgery (January 2001–April 2009, n = 84) were compared to patients who underwent CME/CVL (May 2009–January 2015, n = 71). The primary end point was anastomotic leak. Secondary end points were delayed gastric emptying, severe respiratory failure, mortality and length of hospital stay.
Results
No significant difference was found in the rate of anastomotic leak (1.2% in the conventional versus 5.6% in the CME/CVL group, p = 0.108). Patients in the CME/CVL group had a higher 90-day mortality rate (7.0% versus 0.0%, p = 0.019). Four out of five deceased patients suffered from aspiration with consecutive respiratory failure. There was a tendency towards delayed gastric emptying in the CME/CVL group (12.7% versus 7.1%, p = 0.246). Clavien-Dindo complication grades ≥ 2 were similar in both groups with 16 (19%) in the conventional and 15 (21.1%) in the CME/CVL group ( p = 0.747). CME/CVL patients had a shorter mean length of stay with 11 versus 14 days ( p < 0.001).
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline.
- Record: found
- Abstract: found
- Article: not found
Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial.
- Record: found
- Abstract: found
- Article: not found