- Record: found
- Abstract: found
- Article: found
Does regulation increase the rate at which doctors leave practice? Analysis of routine hospital data in the English NHS following the introduction of medical revalidation
Read this article at
Abstract
Background
In 2012, the UK introduced medical revalidation, whereby to retain their licence all doctors are required to show periodically that they are up to date and fit to practise medicine. Early reports suggested that some doctors found the process overly onerous and chose to leave practice. This study investigates the effect of medical revalidation on the rate at which consultants (senior hospital doctors) leave NHS practice, and assesses any differences between the performance of consultants who left or remained in practice before and after the introduction of revalidation.
Methods
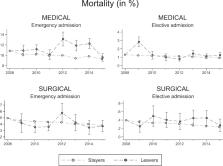
We used a retrospective cohort of administrative data from the Hospital Episode Statistics database on all consultants who were working in English NHS hospitals between April 2008 and March 2009 ( n = 19,334), followed to March 2015. Proportional hazard models were used to identify the effect of medical revalidation on the time to exit from the NHS workforce, as implied by ceasing NHS clinical activity. The main exposure variable was consultants’ time-varying revalidation status, which differentiates between periods when consultants were (a) not subject to revalidation—before the policy was introduced, (b) awaiting a revalidation recommendation and (c) had received a positive recommendation to be revalidated. Difference-in-differences analysis was used to compare the performance of those who left practice with those who remained in practice before and after the introduction of revalidation, as proxied by case-mix-adjusted 30-day mortality rates.
Results
After 2012, consultants who had not yet revalidated were at an increased hazard of ceasing NHS clinical practice (HR 2.33, 95% CI 2.12 to 2.57) compared with pre-policy levels. This higher risk remained after a positive recommendation (HR 1.85, 95% CI 1.65 to 2.06) but was statistically significantly reduced ( p < 0.001). We found no statistically significant differences in mortality rates between those consultants who ceased practice and those who remained, after adjustment for multiple testing.
Conclusion
Revalidation appears to have led to greater numbers of doctors ceasing clinical practice, over and above other contemporaneous influences. Those ceasing clinical practice do not appear to have provided lower quality care, as approximated by mortality rates, when compared with those remaining in practice.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Unskilled and unaware of it: how difficulties in recognizing one's own incompetence lead to inflated self-assessments.
- Record: found
- Abstract: found
- Article: not found
Why is U.K. medicine no longer a self-regulating profession? The role of scandals involving "bad apple" doctors.
- Record: found
- Abstract: not found
- Article: not found