- Record: found
- Abstract: found
- Article: found
Exploring why patients with cancer consult GPs: a 1-year data extraction
Read this article at
Abstract
Background
Survival rates of patients with cancer are increasing owing to improvements in diagnostics and therapies. The traditional hospital-based follow-up model faces challenges because of the consequent increasing workload, and it has been suggested that selected patients with cancer could be followed up by GPs.
The hypothesis of the study was that, regardless of the hospital-based follow-up care, GPs see their patients with cancer both for cancer-related problems as well as for other reasons. Thus, a formalised follow-up by GPs would not mean too large a change in GPs’ workloads.
Design & setting
A 1-year explorative study was undertaken, based on data from 91 Norwegian GPs from 2016–2017.
Results
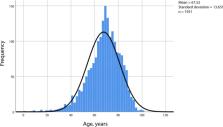
Data were collected from 91 GPs. There were 11 074 consultations in total, generated by 1932 patients with cancer. The mean consultation rate was higher among the patients with cancer compared with Norwegian patients in general. In one-third of the consultations, cancer was the main diagnosis. Apart from cancer, cardiovascular and musculoskeletal diagnoses were common. Patients with cancer who had multiple diagnoses or psychological diagnoses did not consult their GP significantly more often than patients with cancer without such comorbidity.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review.
- Record: found
- Abstract: found
- Article: not found
