- Record: found
- Abstract: found
- Article: found
Empagliflozin prevents doxorubicin-induced myocardial dysfunction
Read this article at
Abstract
Background
Empagliflozin showed efficacy in controlling glycaemia, leading to reductions in HbA1c levels, weight loss and blood pressure, compared to standard treatment. Moreover, the EMPA-REG OUTCOME trial demonstrated a 14% reduction of major adverse cardiovascular events (MACE), a 38% reduction in cardiovascular (CV) death and a 35% reduction in the hospitalization rate for heart failure (HF). These beneficial effect on HF were apparently independent from glucose control. However, no mechanistic in vivo studies are available to explain these results, yet. We aimed to determine the effect of empagliflozin on left ventricular (LV) function in a mouse model of doxorubicin-induced cardiomyopathy (DOX-HF).
Methods
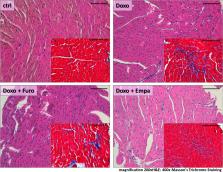
Male C57Bl/6 mice were randomly assigned to the following groups: controls (CTRL, n = 7), doxorubicin (DOX, n = 14), DOX plus empagliflozin (DOX + EMPA, n = 14), or DOX plus furosemide (DOX + FURO group, n = 7). DOX was injected intraperitoneally. LV function was evaluated at baseline and after 6 weeks of treatment using high-resolution echocardiography with 2D speckle tracking (Vevo 2100). Histological assessment was obtained using Haematoxylin and Eosin and Masson’s Goldner staining.
Results
A significant decrease in both systolic and diastolic LV function was observed after 6 weeks of treatment with doxorubicin. EF dropped by 32% (p = 0.002), while the LS was reduced by 42% (p < 0.001) and the CS by 50% (p < 0.001). However, LV function was significantly better in the DOX + EMPA group, both in terms of EF (61.30 ± 11% vs. 49.24 ± 8%, p = 0.007), LS (− 17.52 ± 3% vs. − 13.93 ± 5%, p = 0.04) and CS (− 25.75 ± 6% vs. − 15.91 ± 6%, p < 0.001). Those results were not duplicated in the DOX + FURO group. Hearts from the DOX + EMPA group showed a 50% lower degree of myocardial fibrosis, compared to DOX mice (p = 0.03). No significant differences were found between the DOX + FURO and the DOX group (p = 0.103).
Related collections
Most cited references42
- Record: found
- Abstract: found
- Article: not found
Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications.
- Record: found
- Abstract: found
- Article: not found
Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA).
- Record: found
- Abstract: found
- Article: not found