- Record: found
- Abstract: found
- Article: found
SPIRONOLACTONE FOR NONRESOLVING CENTRAL SEROUS CHORIORETINOPATHY : A Randomized Controlled Crossover Study
Read this article at
Abstract
This study is a randomized controlled crossover study evaluating the effect of spironolactone, a mineralocorticoid receptor antagonist for the treatment of nonresolving central serous chorioretinopathy. Spironolactone significantly reduced both serous retinal detachment and choroidal thickness as compared with placebo. Larger clinical trials are needed to confirm these promising results.
Purpose:
To evaluate the effect of spironolactone, a mineralocorticoid receptor antagonist, for nonresolving central serous chorioretinopathy.
Methods:
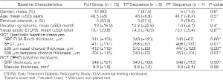
This is a prospective, randomized, double-blinded, placebo-controlled crossover study. Sixteen eyes of 16 patients with central serous chorioretinopathy and persistent subretinal fluid (SRF) for at least 3 months were enrolled. Patients were randomized to receive either spironolactone 50 mg or placebo once a day for 30 days, followed by a washout period of 1 week and then crossed over to either placebo or spironolactone for another 30 days. The primary outcome measure was the changes from baseline in SRF thickness at the apex of the serous retinal detachment. Secondary outcomes included subfoveal choroidal thickness and the ETDRS best-corrected visual acuity.
Results:
The mean duration of central serous chorioretinopathy before enrollment in study eyes was 10 ± 16.9 months. Crossover data analysis showed a statistically significant reduction in SRF in spironolactone treated eyes as compared with the same eyes under placebo ( P = 0.04). Secondary analysis on the first period (Day 0–Day 30) showed a significant reduction in subfoveal choroidal thickness in treated eyes as compared with placebo ( P = 0.02). No significant changes were observed in the best-corrected visual acuity. There were no complications related to treatment observed.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes.
- Record: found
- Abstract: found
- Article: not found
Pachychoroid pigment epitheliopathy.
- Record: found
- Abstract: found
- Article: not found