- Record: found
- Abstract: found
- Article: found
In vivo validation of the adequacy calculator for continuous renal replacement therapies
Read this article at
Abstract
Introduction
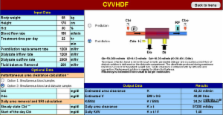
The study was conducted to validate in vivo the Adequacy Calculator, a Microsoft Excel-based program, designed to assess the prescription and delivery of renal replacement therapy in the critical care setting.
Methods
The design was a prospective cohort study, set in two intensive care units of teaching hospitals. The participants were 30 consecutive critically ill patients with acute renal failure treated with 106 continuous renal replacement therapies (CRRT). Urea clearance computation was performed with the Adequacy Calculator ( K CALC). Simultaneous blood and effluent urea samples were collected to measure the effectively delivered urea clearance ( K DEL) at the beginning of each treatment and, during 73 treatments, between the 18th and 24th treatment hour. The correlation between 179 computed and 179 measured clearances was assessed. Fractional clearances for urea were calculated as sp Kt/ V (where sp represents single pool, K is clearance, t is time, and V is urea volume of distribution) obtained from software prescription and compared with the delivered sp Kt/ V obtained from empirical data.
Results
We found that the value of clearance predicted by the calculator was strongly correlated with the value obtained from computation on blood and dialysate determination ( r = 0.97) during the first 24 treatment hours, regardless of the renal replacement modality used. The delivered sp Kt/ V (1.25) was less than prescribed (1.4) from the Adequacy Calculator by 10.7%, owing to therapy downtime.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial.
- Record: found
- Abstract: found
- Article: not found
Acute renal failure in intensive care units--causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure.
- Record: found
- Abstract: found
- Article: not found