- Record: found
- Abstract: found
- Article: found
Combination of Multiple Hemodialysis Modes: Better Treatment Options for Patients Under Maintenance Hemodialysis
Abstract
Purpose
Chronic renal failure has become a major public health concern and treatment strategies are urgently needed. We aimed to investigate whether combination of hemodialysis modes was superior to regular hemodialysis for patients under maintenance hemodialysis.
Patients and Methods
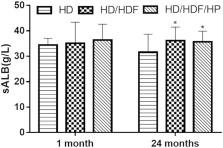
A total of 144 patients with end-stage renal failure (ESRF) were enrolled in this single-center retrospective study. Patients received regular hemodialysis (HD) were included in HD group (n=52), patients received regular HD plus hemodiafiltration (HDF) in HD/HDF group (n=47), patients received the combination of regular HD, HDF and hemoperfusion (HP) in HD/HDF/HP group (n=45). After 1-month and 24-months treatment, therapeutic effects were assessed in terms of nutritional status, control of complications, dialysis adequacy, mean arterial pressure (MAP), infection rate and living quality.
Results
When patients received 1-month treatment, there were no statistically significant differences among three groups. After 24-months treatment, patients in HD/HDF and HD/HDF/HP group presented with better dialysis adequacy, lower MAP and infection rate, higher serum albumin, hemoglobin and calcium levels, lower serum phosphorus and intact parathyroid hormone levels, lower incidence of malnutrition and the Hamilton Depression Scale score, higher the Barthel Index score than HD group ( P<0.05). The levels of calcium, phosphorus and intact parathyroid hormone in HD/HDF/HP group were lower than those in HD/HDF group ( P<0.05).
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Mineral metabolism, mortality, and morbidity in maintenance hemodialysis.
- Record: found
- Abstract: found
- Article: not found
The risk of acute renal failure in patients with chronic kidney disease.
- Record: found
- Abstract: found
- Article: not found