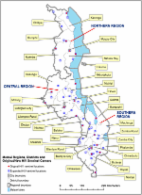
Introduction The Middle East and North Africa (MENA) region has been singled out as the region with little data and where the status of the HIV/AIDS epidemic remained unknown [1]–[8]. In 2005, the region was characterized as “a real hole in terms of HIV/AIDS epidemiological data” [9]. The MENA region has, however, witnessed a remarkable growth in HIV research over the last decade, with several countries developing surveillance systems to monitor the spread of HIV infection, including among most-at-risk populations [10]. A large fraction of studies conducted in the region has remained unpublished in the scientific literature, and only available in the form of difficult to access country reports. This has meant that data have not been analyzed or synthesized at either country or regional level, and no critical assessment of the quality of available evidence has been conducted. The rationale for this study came from signs of a growing HIV disease burden in the MENA region, which highlighted the urgent need for a critical and comprehensive evaluation of the status of the HIV epidemic and of the quality of evidence among the different population groups to inform HIV policy and programming in the region; this was the mandate of the MENA HIV/AIDS Synthesis Project, the largest HIV study in MENA to date [11]. The present article follows on from a series of studies conducted as part of the Synthesis Project. These studies include a high-level overview of HIV epidemiology in MENA [12], a systematic review of HIV molecular evidence [13], and the first documentation of the emerging HIV epidemic among men who have sex with men (MSM) in MENA [14]. The present study is, to our knowledge, the first systematic review and data synthesis to characterize the status of the HIV epidemic among people who inject drugs (PWID) in MENA. The presented regional analysis takes on an additional importance with the need to capture the volume of bio-behavioral surveillance data that became available within the last few years in MENA, and is yet to be analyzed and synthesized within a country-specific or a regional context [15]. PWID are one of the key populations at high risk of HIV in MENA, a region with several vulnerability factors for injecting drug use. For example, 83% of the global supply of heroin is produced in Afghanistan [16], and over 75% of this is trafficked through Iran and Pakistan. In 2009, Iran bore the highest fraction of the global opium and heroin seizures (89% and 33%, respectively) [16]. Increased availability and purity of heroin at lower prices in MENA appears to have led to a subsequent rise in injecting drug use [17]. In 2010, one gram of heroin in Afghanistan could be purchased for about US$4 compared with up to US$100 in West and Central Europe, US$200 in the United States and Northern Europe, and US$370 in Australia [16]. Most PWID in the region are young adults and marginalized by family members and society; they are stigmatized and lack access to comprehensive and confidential HIV prevention and treatment services [11]. The primary objective of this study was to assess the status of the HIV epidemic among PWID in MENA by describing HIV prevalence and incidence. The secondary objective was to describe the risk behavior environment and the HIV epidemic potential among PWID by describing (1) their injecting and sexual risk behavior and knowledge, and (2) prevalence of proxy biological markers of these behaviors, namely hepatitis C virus (HCV) and sexually transmitted infections (STIs), respectively. The study also estimated the proportion and number of PWID in MENA. Methods We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Text S1) [18],[19] and Cochrane Collaboration guidelines [20]. Data Sources and Search Strategy Our review covered the 23 countries included in the MENA definitions of the three international organizations leading the regional HIV response efforts in the region: the Joint United Nations Programme on HIV/AIDS (UNAIDS), the Eastern Mediterranean Regional Office of the World Health Organization (WHO/EMRO), and the World Bank (Figure 1). These countries share specific similarities, whether historical, socio-cultural, or linguistic; and are conventionally included together as part of HIV/AIDS programming for the region. 10.1371/journal.pmed.1001663.g001 Figure 1 Map of the Middle East and North Africa region. The defintion adopted in the review includes the following 23 countires: Afghanistan, Algeria, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, OPT, Pakistan, Qatar, Saudi Arabia, Somalia, Sudan (including the newly established Republic of South Sudan), Syria, Tunisia, United Arab Emirates (UAE), and Yemen. The following sources of data were searched up to December 16, 2013: (1) Scientific databases (PubMed, Embase, and regional databases [WHO African Index Medicus [21] and WHO Index Medicus for the Eastern Mediterranean Region [22]]), with no publication date or language restrictions. A generic search of “drug use” in MENA was performed in PubMed and Embase using MeSH/Emtree and text terms. The term “HIV” was not included to avoid detection bias. (2) The MENA HIV/AIDS Synthesis Project database of grey and mainly unpublished literature [11],[12]. (3) Abstracts of the International AIDS Conference 2002–2012 [23], the International AIDS Society Conference on HIV Pathogenesis and Treatment 2001–2013 [24], and the International Society for Sexually Transmitted Diseases Research Conferences 2003–2013 [25]. (4) International and regional databases of HIV prevalence measures including the US Census Bureau database of HIV/AIDS [26], the WHO/EMRO HIV testing database [27], and the UNAIDS epidemiological fact sheets database [28]. Details of the search criteria are provided in Text S2. Reference lists of all relevant papers and review articles were also searched. Study Selection Titles and abstracts of all records identified were screened independently by two authors (GRM and SR), and consensus on potential eligibility reached. Full texts of potentially relevant records were retrieved and assessed for eligibility. Studies satisfying any of the below criteria were eligible: (1) The proportion of PWID in the sample was specified, at least half were PWID, and data on any of the following outcomes were included: Prevalence or incidence of HIV; prevalence of injecting or sexual risk behaviors, or knowledge; prevalence or incidence of HCV; and prevalence or incidence of other STIs. HCV is transmitted primarily through percutaneous exposures and can be used as a proxy of the risk of parenteral exposure to HIV. Among PWID, a threshold HCV prevalence of about 30% implies sufficient risk behavior to sustain HIV transmission [29],[30]. Similarly, the prevalence of STIs is a useful marker of sexual risk behavior and potential for HIV sexual acquisition. (2) Data on population-based prevalence of injecting drug use or PWID population size estimates were reported. Only studies with primary data were included. The only exception was in relation to national estimates of the number and proportion of PWID in a number of MENA countries where the only available source of data was from two global reviews [4],[31] that published data compiled through the Reference Group to the UN on HIV and Injecting Drug Use [32]. We used the term report to refer to the documents (papers, conference abstracts, or public health reports) presenting findings of a study [20]. Reports could contribute to more than one outcome. Findings duplicated in more than one report were included only once (using the more detailed report). Outcomes in more than one population/setting within a report were included separately. Data Extraction Data were extracted by one of the authors (GRM) using a pre-piloted data extraction form and entered into a computerized database. Double extraction on about 45% of records was confirmed by another author (LA-R). The few discrepancies were settled by consensus or by contacting authors. Data from articles in English, French, and Arabic were extracted from the full -texts. Data from records in Farsi (n = 6) were extracted from the English abstract. There were no records in other languages. As supporting information, we also analyzed data extracted from countries' reporting on the HIV epidemic to WHO/EMRO in the format of aggregate HIV case notifications. Scope and Quality of the Evidence We appraised the status of the evidence on our main outcome, HIV prevalence, at country level by examining the following criteria that take into consideration the quantity, quality, and geographical coverage of available data: (1) the number of HIV prevalence measures and the total sample size they cover, (2) the number of geographic settings with HIV prevalence measures, (3) the number of multi-city studies and the maximum number of cities per study, (4) the number of rounds of integrated bio-behavioral surveillance surveys (IBBSS), and (5) the quality and precision of individual HIV prevalence measures. The quality of individual HIV prevalence measures was assessed by describing the risk of bias (ROB). Since the number of prevalence measures among female PWID was very small and often based on small sub-samples, the quality appraisal was restricted to HIV prevalence among predominantly male PWID. Based on the Cochrane approach for assessing ROB [20], we classified each HIV prevalence measure as having a low, high, or unclear ROB for three quality domains: the sampling methodology, the type of HIV ascertainment, and the response rate. Low ROB was considered if (1) sampling was probability-based or preceded by ethnographic mapping, (2) HIV was ascertained with a biological assay, and (3) the response rate was over 80%; or over 80% of the target sample size was reached. HIV prevalence measures extracted from international and regional databases were considered of unknown quality since original reports were not available for assessing their ROB. A minimum sample size of 100 was considered to produce estimates with good precision. For a median HIV prevalence among PWID in MENA of 8% (see Results), this implies a 95% CI of 4%–15%. The quality of the evidence in each country was assessed by combining the above factors as described in Text S3. For example, quality was considered better if at least one round of IBBSS was conducted, since these surveys use standard methodology including state of the art sampling techniques of hard-to-reach populations (such as respondent-driven sampling). Countries were categorized as having: (1) No evidence: virtually no data. (2) Poor evidence: The majority of HIV biological measures were of poor quality. (3) Limited evidence: The number of HIV biological measures was small, but of reasonable quality. (4) Good evidence: The number of HIV biological measures was small, but with good quality and informative data. However, the overall volume of data was not sufficient to be conclusive of the status and scale of the epidemic at the national level. (5) Conclusive evidence: There was a sufficient volume of robust evidence to support the conclusion. Analysis The low-bound, middle, and high-bound national estimates of the number and prevalence of injecting drug use in MENA countries were extracted from reports. The pooled number and prevalence of PWID for the MENA region were estimated separately using the extracted country-level estimates. The lower (and upper) bound of our pooled regional estimate of the number of PWID in MENA was calculated by adding the lowest (and highest) reported number of PWID in all MENA countries. The middle figure for the number of PWID in MENA is the sum of the middle estimates in each of the MENA countries. When more than one such estimate was available per country, we used the median of the estimates. The pooled numbers of PWID were rounded up to the next thousand. Middle estimates of the extracted prevalence of PWID were weighted by adult population size to derive the pooled prevalence of injecting drug use in MENA. When more than one such estimate was available per country, we used the median of the estimates. Adult population size was extracted from the United Nations World Population Database [33]. Sub-national estimates of the number and prevalence of injecting drug use were extracted from reports and described separately. We calculated 95% CI for HIV and HCV prevalence for all reports with available information. The HIV biological data (HIV prevalence from reports and from databases, HIV incidence, and notified HIV cases) were synthesized at country level to assess the status of the HIV epidemic among PWID. Recent WHO/UNAIDS guidelines for classifying HIV epidemics [34],[35], which do not recommend use of rigid thresholds [34],[36], were adapted to classify the HIV epidemic level in PWID as: (1) Low-level HIV epidemic: HIV has not reached significant levels among PWID. (2) Concentrated HIV epidemic: HIV has reached significant levels and taken root among PWID through transmission chains between members of this population. Concentrated epidemics can be either emerging (HIV has started its initial growth and continues in a trend of increasing HIV prevalence); or established (the epidemic has reached its peak and HIV prevalence is stabilizing towards, or already is at, its endemic level). (3) “At least outbreak-type”: Insufficient evidence to support a concentrated epidemic among PWID, but some evidence, usually of lower quality, suggesting that significant HIV transmission has occurred, or is occurring, among at least some PWID groups. The terms “national” or “at least localized” were assigned to concentrated epidemics to reflect the geographical spread of the epidemic within a given country. Results Results of Search Strategy The study selection process is shown in Figure 2. A total of 6,207 citations were retrieved from PubMed, Embase, and the regional databases. After full-text screening and including reports from the other sources, 192 reports were eligible: 121 from PubMed and Embase, 41 from the MENA HIV/AIDS Synthesis Project, 13 from bibliographies of relevant reports and review articles, 13 from the search of scientific conferences, and four from the regional databases. In addition, 226 HIV point-prevalence measures were extracted from the databases of biological markers (Figure 2). 10.1371/journal.pmed.1001663.g002 Figure 2 PRISMA flow chart of study selection in the systematic search. There were 423 HIV prevalence measures, 197 of which were extracted from the eligible reports and 226 from the databases of HIV prevalence; three HIV incidence measures; 93 HCV prevalence measures; four HCV incidence measures; 38 STI prevalence measures; and 993 behavioral and knowledge measures. There were also 130 and 96 measures on the number and proportion of PWID, respectively (Figure 2). Scope and Quality of the Evidence The number and quality of HIV prevalence measures varied by country. The largest volume of data was from Pakistan (101 HIV prevalence measures on a total of 24,445 PWID), Iran (99 HIV prevalence measures on a total of 22,181 PWID), and Egypt (39 HIV prevalence measures on a total of 4,480 PWID) (Table 1). A smaller number of HIV prevalence measures but covering a relatively large number of PWID were conducted in Afghanistan (3,277 PWID), Tunisia (1,522 PWID), and Morocco (880 PWID). Multi-city studies have been conducted in several countries including Pakistan, where up to 16 cities were included in one study [37]. IBBSS have been conducted in Afghanistan [38],[39], Egypt [40]–[42], Iran [43],[44], Jordan [45], Lebanon [46], Libya [47], Morocco [48], Occupied Palestinian Territories (OPT) [49], Pakistan [37],[50]–[52], and Tunisia (Table 1) [53],[54]. Pakistan has the most repeated rounds of IBBSS with four rounds conducted between 2005 and 2011 [37],[50]–[52]. 10.1371/journal.pmed.1001663.t001 Table 1 Summary of the HIV biological evidence per country. Biological Evidence Afg Alg Bah Dji Egy Irn Irq Jor Kuw Leb Lib Mor Oma OPT Pak Qat SA Som Sud Syr Tun UAE Yem Number HIV biological studies a 5 — 1 — 7 47 — 1 — 2 1 3 1 1 27 — — — — 1 2 — — Number HIV prevalence measures 19 — 23 6 39 99 7 13 17 8 4 21 17 4 101 — 7 — 1 22 10 — 5 From reports (total sample size) 13 (3,277) — 1 (242) — 9 (4,480) 78 (22,181) — 3 (227) — 2 (121) 1 (328) 5 (880) 3 (135) 1 (199) 77 (24,445) — — — — 1 (204) 3 (1,522) — — From databases 6 — 22 6 30 21 7 10 17 6 3 16 14 3 24 — 7 — 1 21 7 — 5 Number HIV incidence measures a 1 — — — 1 — — — — — — — 1 — — — — — — — — Number cities/provinces with HIV prevalence measures a 6 — 1 — 2 27 — 3 — 1 1 4 1 1 26 — — — — 1 3 — — Number multi-city studies (max number cities/study) a 3 (5) — — — 1 (2) 4 (10) — 1 (4) — — — 2 (2) — — 12 (16) — — — — — 2 (3) — — Number repeated IBBSS a 2 — — — 2 2 — 1 — 1 1 1 — 1 4 — — — — — 2 — — a With reports available. Afg, Afghanistan; Alg, Algeria; Bah, Bahrain; Dji, Djibouti; Egy, Egypt; Irn, Iran; Irq, Iraq; Jor, Jordan; Kuw, Kuwait; Leb, Lebanon; Lib, Libya; Mor, Morocco; Oma, Oman; Pak, Pakistan; QA, Qatar; SA, Saudi Arabia; Som, Somalia; Sud, Sudan; Syr, Syria; Tun, Tunisia; UAE, United Arab Emirates; Yem, Yemen. Of 190 HIV prevalence measures extracted from eligible reports and among predominantly male PWID, 98%, 53%, and 34% had low ROB in terms of HIV ascertainment, sampling methodology, and response rate, respectively. Over 60% of the 190 HIV prevalence measures had low ROB in at least two quality domains and 84% had good precision (Tables S1 and S2). On the basis of the quality of the evidence assessment, the evidence was determined to be “conclusive” in Iran and Pakistan; “good” in Afghanistan, Egypt, Jordan, Lebanon, Libya, Morocco, OPT, and Tunisia; “limited” in Bahrain and Syria; and “poor” in Djibouti, Iraq, Kuwait, Oman, Saudi Arabia, Sudan, and Yemen. There was “no evidence” in Algeria, Qatar, Somalia, and the United Arab Emirates. A narrative justification for the classification of the scope and quality of evidence is in Text S3. Although a formal quality assessment was not made for the secondary outcomes in terms of injecting and sexual risk behavior and knowledge, the majority of these data were extracted from the IBBSS studies using standard survey methodology and large samples. Details of these studies (with information on sample size, population characteristics, and/or sampling technique) can be found in the tables summarizing the prevalence of HIV and HCV among PWID (Tables 3 and 6). Prevalence of Injecting Drug Use Table 2 describes national estimates of the number and prevalence of PWID. These national estimates were extracted from included reports where they were derived using different methodologies including indirect methods (such as capture-recapture and multiplier methods), population-based surveys, registered number of PWID, and rapid assessments. In two of the sources of data in Table 2 [4],[31], some of the country estimates are the collation of several such country-specific estimates using methods described in the original reports [4],[31]. 10.1371/journal.pmed.1001663.t002 Table 2 National estimates of the number and prevalence of people who inject drugs in the Middle East and North Africa as extracted from included reports. Country Population 15–64 Years [33] Year of Estimate PWID Estimate (Number) PWID Prevalence (%) Source Low Middle High Low Middle High Afghanistan 16,119,000 a 22,720 34,080 45,440 0.16 0.24 0.32 [4] 2005 6,870 6,900 6,930 0.05 0.05 0.05 [31] 2009 18,000 20,000 23,000 [124] 2009 0.11 [125] Algeria 24,246,000 a 26,333 40,961 55,590 0.14 0.22 0.29 [4] Bahrain 983,000 a 337 674 1,011 0.08 0.16 0.24 [4] Djibouti — — — — — — — — Egypt 51,460,000 a 56,970 88,618 120,265 0.13 0.21 0.28 [4] Iran 53,132,000 a 70,000 185,000 300,000 0.17 0.46 0.74 [4] 2004 180,000 0.40 [31] 2007 250,000 [126] Iraq 16,967,000 a 23,115 34,673 46,230 0.19 0.28 0.37 [4] Jordan 3,624,000 a 3,200 4,850 6,500 0.11 0.16 0.22 [4] Kuwait 1,937,000 a 2,700 4,100 5,500 0.20 0.30 0.41 [4] Lebanon 2,871,000 a 2,200 3,300 4,400 0.09 0.14 0.19 [4] Libya 4,148,000 a 4,633 7,206 9,779 0.15 0.23 0.32 [4] 2001 1,685 0.05 [31] Morocco 21,247,000 a 18,500 0.10 [4] Oman 1,956,000 a 2,800 4,250 5,700 0.20 0.30 0.40 [4] OPT 2,212,000 a 1,200 1,850 2,500 0.22 0.35 0.47 [4] Pakistan 104,724,000 a 54,000 462,000 870,000 0.07 0.50 1.12 [4] 2006 125,000 130,460 150,000 0.13 0.14 0.16 [31] 2006 102,042 0.25 [57] 2010 99,000 [126] Qatar 1,503,000 a 780 1,190 1,600 0.15 0.22 0.30 [4] Saudi Arabia 18,306,000 a 15,172 23,600 32,028 0.13 0.20 0.27 [4] 2008 10,000 [126] Somalia 4,885,000 a 1,000 0.03 [4] Sudan 24,540,000 a 24,319 37,828 51,337 0.13 0.20 0.28 [4] Syria 12,073,000 a 4,000 6,000 8,000 0.04 0.07 0.09 [4] Tunisia 7,294,000 a 8,462 13,163 17,864 0.14 0.21 0.29 [4] 2009 9,000 [126] UAE 6,200,000 a 3,200 4,800 6,400 0.20 0.30 0.40 [4] Yemen 12,800,000 a 12,710 19,770 26,830 0.15 0.23 0.31 [4] a The specific year of the estimate was not mentioned in the original report, but the report covered data from 1998–2005. UAE, United Arab Emirates. Based on available data, the number of PWID in MENA ranges between a low bound of 335,000 and a high bound of 1,635,000, with a middle estimate of 626,000 PWID. Iran, Pakistan, and Egypt have the largest number, with a median of about 185,000, 117,000, and 89,000 PWID, respectively. The weighted mean prevalence of injecting drug use in MENA is 0.24 per 100 adults. It is lowest in Somalia (0.03%) and highest in Iran (0.43%) (Table 2). Studies of sub-national populations showed geographical heterogeneity (Table S3). For example, in Iran, the prevalence of injecting drug use varied between 0.0% in rural Babol province [55] to 1.0% in Tehran [56]; and in Pakistan it ranged from 0.02% in Rawalpindi to 0.87% and 1.07% in Sargodha and Faisalabad, respectively [57]. Data on the prevalence of female PWID in MENA were scarce. Overall, the mean proportion of females among PWID in included studies was 2.3% (range: 0%–35%). In two studies in Oman and Syria, 25%–58% [58] and 48% [59] of PWID, respectively, reported knowing at least one female PWID. HIV Prevalence, Incidence, and Mode of Transmission HIV prevalence measures from reports and databases are summarized in Tables 3 and S4, respectively. Considerable variation in HIV prevalence was seen, with an overall median of 8% (interquartile range [IQR]: 1%–21%) (Table 3). HIV prevalence among PWID in MENA ranged between 0% in some prevalence measures in almost every country up to 7% in Cairo, Egypt in 2010 (n = 274) [42]; 18% in Afghanistan in one city near the Iranian borders, Herat, in 2009 (n = 159) [38]; 21% in Manama, Bahrain, in the early nineties (n = 242) [60]; 27% in Oman among incarcerated PWID (n = 33) [58]; 38% in Nador, northern Morocco, in 2008 (n = 233) [61]; 52% in the third largest metropolis in Pakistan, Faisalabad, in 2011 (n = 364) [37]; 72% in rural Iran in 2004–5 (n = 61) [62]; and 87% in Tripoli, Libya in 2010 (n = 328) [47] (Table 3). HIV prevalence was consistently low among PWID in Jordan, Lebanon, OPT, Syria, and Tunisia (0%–3.1%). Substantial intra-country variability in HIV prevalence was observed in Afghanistan, Iran, Morocco, and Pakistan (Table 3). In most countries with high HIV prevalence, recent studies report increasing HIV prevalence starting around 2003 (Tables 3 and S4). 10.1371/journal.pmed.1001663.t003 Table 3 HIV prevalence among people who inject drugs in the Middle East and North Africa as extracted from reports included in the systematic review. Country Citation Year City Study Site Sampling Population Sample Size HIV Prevalence Percent 95% CI Afghanistan MOH, 2012 [39] (Round II) 2012 Herat RDS All male 185 13.3a 8.9–19.3 Kabul RDS All male 369 2.4a 1.1–4.6 Mazar-i-Sharif RDS All male 254 0.3a 0.0–2.2 Jalalabad RDS All male 236 1.0a 0.1–3.0 Charikar RDS All male 117 0.9a 0.0–4.7 MOH, 2010 [38] (Round I) 2009 Herat RDS All male 159 18.2 12.6–25.1 Kabul RDS All male 286 3.2 1.4–5.9 Mazar-i-Sharif RDS All male 102 1.0 0.0–5.3 Todd, 2011 [69] 2007–2009 Kabul Harm reduction center & community CS All male 483 2.1 1.0–3.8 Nasir, 2011 [127] 2006–2008 Herat VCT CS 99% male 340 3.2 1.6–5.7 Jalalabad VCT CS 99% male 96 0.0 — Mazar-i-Sharif VCT CS 99% male 187 0.0 — Todd, 2007 [128] 2005–2006 Kabul VCT CS All male 463 3.0 1.7–5.0 Bahrain Al-Haddad, 1994 [60] 1991 Manama Voluntary drug treatment center CS All male 242 21.1 16.1–26.8 Egypt MOH/FHI, 2010 [42] (Round II) 2010 Alexandria RDS All male 284 6.5a 3.3–10.3a Cairo RDS All male 274 6.8a 3.9–10.8a Elghamrawy, 2012 [129] 2008–2011 Cairo Harm reduction center CS All male 3,222 1.4 1.0–1.9 Soliman, 2010 [41] (Round I) 2006 Cairo RDS All male 413 0.6a 0.1–1.8a MOH/FHI, 2006 [40] (Round I) 2006 Cairo RDS All female 16 0.0 — Saleh, 1998 [130] 1994 Alexandria Voluntary drug treatment center CS 100 0.0 — Attia, 1996 [131] — Alexandria Voluntary drug treatment center CS 54 0.0 — Hasan, 1994 [132] — CS 79 7.6 2.8–15.8 El-Ghazzawi, 1987 [133] — Alexandria CS 38 0.0 — Iran Honarvar, 2013 [134] 2012–2013 Shiraz Voluntary drug treatment center CS 98% male 233 7.7 4.6–11.9 Mehrejredi, 2013 [135] 2011 Tehran VCT and harm reduction center CS 91% male 209 2.9 1.1–6.1 MOH, 2010 [44] (Round II) 2010 Fars VCT, Harm reduction center, voluntary drug treatment center, & community CS 98% male 250 31.9 26.3–38.2 Lorestan Idem CS All male 222 26.4 20.9–32.9 Tehran Idem CS 95% male 567 23.9 20.5–27.7 Sistan & Baluchestan Idem CS 99% male 138 18.3 12.1–25.6 Kermanshah Idem CS 99% male 249 16.8 12.4–22.1 Khouzestan Idem CS 99% male 198 9.4 5.9–14.6 Mazandaran Idem CS 97% male 276 7.0 4.2–10.5 Kerman Idem CS 94% male 213 6.2 3.3–10.2 Azerbaijan Sharghi Idem CS 100% male 118 3.6 0.9–8.5 Khorasan Razavi Idem CS 99% male 248 2.2 0.7–4.6 Alipour, 2012 [79] 2010 Tehran, Shiraz, & mashhad Harm reduction center CS All male, heterosexually active 226 9.4 5.8–13.9 Tehran, Shiraz, & mashhad Harm reduction center CS All female, sexual partners of PWID 42 7.7 1.5–19.5 Ilami, 2010 [136] 2009–2010 Kohgiloyeh & Boyerahmad CS 158 9.9 5.9–15.9 Hashemepour, 2013 [137] 2009 North Isfahan Community CS 82 1.2 0.0–6.6 South Isfahan Community CS 589 1.0 0.4–2.2 West Isfahan Community CS 479 1.7 0.7–3.3 East Isfahan Community CS 113 3.5 1.0–8.8 Isfahan city Community CS 336 1.5 0.5–3.4 Dibaj, 2013 [138] 2008–2009 Isfahan Prison CS All male 970 6.4 4.9–8.1 Javadi, 2013 [139] 2008–2009 Isfahan Harm reduction center CS 95% male 539 1.1 0.4–2.4 Eskandarieh, 2013 [140] 2008 Tehran Mandatory drug treatment center CS 97% male 258 18.8 14.4–24.3 Zamani, 2010 [141] 2008 Isfahan RDS 98% male 117 0.7a 0·6–2.3a Ghasemian, 2011 [142] 2007–2009 Sari Clinical setting CS 88 18.2 10.8–27.8 Zadeh, 2014 [143] 2007–2008 Tehran Prison CS 3,044 3.7 3.1–4.4 SeyedAlinaghi, 2013 [144] 2007–2008 Tehran Community CS Beggars 658 2.4 1.4–3.9 Kazerooni, 2010 [67] 2007 Shiraz Prison SRS All male 363 6.6 4.3–9.7 Aminzadeh, 2007 [145] 2007 Tehran Clinical setting CS 70 30.0 19.6–42.1 Rahimi_Movaghar, 2010 [146] 2006–2007 Tehran Voluntary drug treatment center & community CS All female 38 10.5 2.9–24.8 Tehran Voluntary drug treatment center & community CS All male 861 10.7 8.7–12.9 Kheirandish, 2010 [147] 2006 Tehran Mandatory drug treatment center CS All male 459 24.4 20.5–28.6 MOH, 2008 [43] (Round I) 2006–2007 Azerbaijan Sharghi Harm reduction center, voluntary drug treatment center, & community TLS 96% male 294 8.2 5.3–11.9 Fars Idem TLS 92% male 353 24.7 20.2–29.5 Kerman Idem TLS 96% male 162 20.8 15.0–28.1 Kermanshah Idem TLS 99% male 259 30.5 25.0–36.5 Khorasan Razavi Idem TLS 98% male 399 6.5 4.3–9.4 Khuzestan Idem TLS 99% male 168 4.2 1.7–8.4 Lorestan Idem TLS 97% male 196 35.7 29.0–42.9 Mazandaran Idem TLS All male 216 11.6 7.6–16.6 SIstan Idem TLS 93% male 142 2.1 0.4–6.0 Tehran Idem TLS 98% male 664 14.4 11.9–17.4 Malekinejad, 2008 [148] 2006–2007 Tehran RDS 98% male 548a 25.0 18.0–28.3 Alavi, 2012 [149] 2005–2006 Ahfaz Voluntary drug treatment center & prison CS All male 109 47.7 38.1–57.5 Ghanbarzadeh, 2006 [150] 2005 Birjand Prison CS All female 10 0.0 — Tofigi, 2011 [151] 2004 Tehran Clinical setting CS Cadavers 400 6.3 4.1–9.1 Imani, 2008 [152] 2004 Shahr-e-Kord Voluntary drug treatment center CS All male 133 0.8 0·0–4·1 Mojtahedzadeh, 2008 [62] 2004–2005 Rural Northwestern Iran Voluntary drug treatment center CS 98% male, rural population 61 72.1 59.2–82.9 Zamani, 2006 [102] 2004 Tehran Harm reduction center & community CS All female 6 33.3 4.3–77.7 Tehran Harm reduction center & community CS All male 207 23.2 17.6–29.5 Shamaei, 2009 [153] 2003–2006 Tehran Clinical setting CS 98% male, TB infected PWID 35 45.7 28.8–63.4 Pourahmad, 2007 [154] 2003 Isfahan, Chaharmahal Bakhtiary, & Lorestan Prison CS All male 401 14.0 10.7–17.7 Zamani, 2005 [155] 2003–2004 Tehran Voluntary drug treatment center CS All female 5 20.0 0.5–71.6 Tehran Voluntary drug treatment center CS All male 165 15.2 10.1–21.5 Farhoudi, 2003 [156] 2003 Karaj Resident prisoners CS All male, resident inmates 371 24.0 19.7–28.7 Karaj Newly admitted prisoners CS All male, newly 7–admitted inmates 369 22.0 17.8–26.5 Khodadadizadeh, 2003 [157] 2003 Rafsanjan Clinical setting CS 96% male 31 9.7 2.0–25.8 Alavi, 2010 [158] 2002–2006 Ahfaz Clinical setting CS 97% male, hospitalized for ID 333 18.0 14.6–23.2 Davoodian, 2009 [159] 2002 Hormozgan Prison SRS 249 15.1 11.0–20.3 Behnaz, 2007 [160] 2002–2003 Gorgan Prison SRS 22 18.2 5.2–40.3 Asadi, 2006 [68] 2002–2004 Tehran Clinical setting CS 98% male 126 35.7 27.4–44.7 Alizadeh, 2005 [161] 2002 Hamadan Prison SRS 93% male 149 0.7 0.0–3.7 Mir Nasseri, 2011 [162] 2001–2002 Tehran Voluntary drug treatment center CS 97% male 90 7.8 3·7–13·5 Tehran Prison SRS 87% male 371 17.0 13.5–21.2 Sharif, 2009 [163] 2001–2006 Kashan Clinical setting CS All female, hospitalized for ID 23 0.0 — Kashan Clinical setting CS All male, hospitalized for ID 177 1.6 0.4–4.9 Alavi, 2009 [164] 2001–2006 Ahfaz Clinical setting CS 92% male 142 12.7 7.7–19.3 Alavi, 2007 [165] 2001–2003 Ahfaz Clinical setting CS All male 154 67.5 59.5–74.8 Rahbar, 2004 [166] 2001–2002 Mashhad Voluntary drug treatment center CS 222 0.0 — Mashhad Prison CS 101 6.9 2.8–13.8 Sharifi-Mood, 2006 [167] 2000–2005 Zahedan Clinical setting CS 97% male, hospitalized for ID 31 25.8 11.9–44.6 Mirahmadizadeh, 2004 [168] 1998 Shiraz Voluntary drug treatment center CS 464 1.2 0.5–2.8 Nowroozi, 1998 [169] 1996 Tehran Prison SRS All male 400 0.0 — Alavian, 2013 [170] — Shiraz Voluntary drug treatment center CS 98% male 144 41.7 33.5–50.2 Azarkar, 2010 [171] — Birjand Prison SRS 17 0.0 — Mirahmadizadeh, 2009 [172] — National National RCS 96% male 936 20.5 18.0–23.2 Amini, 2005 [173] — Tehran Voluntary drug treatment center CS 34 8.8 1.9–23.7 Alaei, 2002 [174] — Kermanshah CS 429 19.2 15.5–23.2 Jordan NAP, 2010 [45] (Round I) 2009 Amman RDS 133 0.0 — Aqaba RDS 78 0.0 — Irbid RDS 16 0.0 — Lebanon Mahfoud, 2010 [46] (Round I) 2007–2008 Beirut RDS All male 81 0.0 — Ramia, 2003 [175] 2000–2002 Beirut Clinical setting CS 75% male 40 0.0 — Libya Mirzoyan, 2013 [47] (Round I) 2010 Tripoli RDS 328 87.1a 81.5–91.9a Morocco MOH, 2012 [117] (Round I) 2011–2002 Nador RDS 99% male 277 25.1a 16.1–35.0 MOH, 2012 [117] (Round I) 2010–2001 Tanger RDS 98% male 261 0.4 0.0–2.1 MOH, 2010 [61] 2008 Al Hoceima RDS 0.0 — Nador RDS 233 37.8 31.5–44.3 Elmir, 2002 [176] 1991–1999 National CS 109 33 24–43 Oman MOH, 2006 [58] — Muscat Voluntary drug treatment center CS All male 17 12b 2–36 — Muscat Prison CS All male 33 27b 13–46 — Muscat Community SBS All male 85 18b 10–27 OPT MOH, 2010 [177] (Round I) 2010 Al Azaria - East Jerusalem RDS 98.5% male 199 0.0 — Pakistan NAP, 2011 [37] (Round IV) 2011 D G Khan Community MSCS 98.4% male 365 49.6 44.3–54.8 Faisalabad Community MSCS 98.4% male 364 52.5 47.2–57.7 Gurjat Community MSCS 98.4% male 208 46.2 39.2–53.2 Lahore Community MSCS 98.4% male 367 30.8 26.1–35.8 Multan Community MSCS 98.4% male 365 24.9 20.6–29.7 Pakpattan Community MSCS 98.4% male 365 3.3 1.7–5.7 Rahim Yar Khan Community MSCS 98.4% male 214 14.9 10.5–20.4 Sarghoda Community MSCS 98.4% male 365 40.6 35.5–45.8 Dadu Community MSCS 98.4% male 194 16.0 11.1–21.9 Karachi Community MSCS 98.4% male 365 42.2 37.1–47.4 Larkana Community MSCS 98.4% male 365 18.6 14.8–23.0 Sukkur Community MSCS 98.4% male 365 19.2 15.3–23.6 Haripur Community MSCS 98.4% male 65 7.9 2.5–17.0 Peshawar Community MSCS 98.4% male 260 20.0 15.3–25.4 Quetta Community MSCS 98.4% male 365 7.1 4.7–10.3 Turbat Community MSCS 98.4% male 365 21.4 17.3–25.9 Nai Zindagi, 2009 [66] 2009 Gurjanwala Community CS 300 8 5–12 Mandi Bahauddin Community CS 300 52 46–58 Rawalpindi Community CS 300 23 18–28 Sheikhukupura Community CS 300 21 17–26 Nai Zindagi, 2008 [89] 2008 Faisalabad CS All male, married 104 13 8–22 Lahore CS All male, married 103 10 5–17 Sarghoda CS All male, married 252 41 35–47 NAP, 2008 [50] (Round III) 2008 D G Khan Community MSCS 99.8% male 345 18.6 14.6–23.1 Faisalabad Community MSCS 99.8% male 400 12.3 9.2–15.9 Hyderabad Community MSCS 99.8% male 397 30.5 26.0–35.3 Karachi Community MSCS 99.8% male 403 23.1 19.1–27.5 Lahore Community MSCS 99.8% male 401 14.5 11.2–18.3 Larkana Community MSCS 99.8% male 389 28.5 24.1–33.3 Peshawar Community MSCS 99.8% male 231 12.8 8.9–18.0 Sarghoda Community MSCS 99.8% male 403 22.8 18.8–27.2 Platt, 2009 [178] 2007 Rawalpindi RDS 98% male 302 2.6 1.2–5.2 Abotabad RDS 98% male 102 0.0 — NAP, 2006–2007 [51] (Round II) 2006–2007 Bannu Community MSCS 72 1.4 0.0–7.5 Faisalabad Community MSCS 400 13.3 10.1–17.0 Gurjanwala Community MSCS 400 1.0 0.3–2.5 Hyderabad Community MSCS 400 29.8 25.3–34.5 Karachi Community MSCS 399 30.1 25.6–34.8 Lahore Community MSCS 400 6.5 4.3–9.4 Larkana Community MSCS 399 16.5 13.0–20.6 Multan Community MSCS 400 0.0 — Peshawar Community MSCS 180 2.2 0.6–5.6 Quetta Community MSCS 190 9.5 5.7–14.6 Sarghoda Community MSCS 400 51.3 46.2–56.2 Sukkur Community MSCS 399 5.3 3.3–7.9 Rahman, 2006 [179] 2005 Lahore CS All male 0.0 — Nai zindagi, 2005 [180] 2005 Faisalabad SRS All male 200 9.5 5.8–14.4 Lahore SRS All male 200 2.5 0.8–5.7 Sarghoda SRS All male 100 12.0 6.4–20.0 Sialkot SRS All male 100 1.0 0.0–5.4 NAP, 2005 [52] (Round I) 2005 Faisalabad Community TLS 400 13.3 10.1–17.0 Hyderabad Community TLS 398 25.3 21.2–30.0 Lahore Community TLS 400 3.8 2.1–6.1 Multan Community TLS 400 0.3 0.0–1.4 Peshawar Community TLS 284 0.4 0.0–1.9 Quetta Community TLS 147 9.5 5.3–15.5 Sukkur Community TLS 402 19.2 15.4–23.3 Bokhari, 2007 [83] 2004 Karachi Community TLS All male 402 23.1 19.1–27.6 Lahore Community TLS All male 397 0.5 0.1–1.8 Achakzai, 2007 [181] 2004 Quetta Community CS 50 24.0 13.1–38.2 Bokhari, 2006 [182] (Pilot) 2004–2005 Karachi TLS 400 26.0 21.8–30.6 Rawalpindi CS 199 0.5 0.0–2.8 Abbasi, 2005 [183] 2004 Larkana VCT CS All male, homeless 3154 8.3 7.4–9.3 Abbasi, 2009 [184] 2003 Quetta Voluntary drug treatment center CS All male 300 0.3 0.0–1.8 Altaf, 2007 [74] 2003 Karachi Harm reduction center CS All male, 80% homeless 161 0.6 0.0–3.4 Kuo, 2006 [70] 2003 Lahore Harm reduction center CS All male 255 0.0 — Quetta Harm reduction center CS 98% male 96 0.0 — Shah, 2004 [185] 2003 Larkana CS 175 9.7 5.8–15.1 Altaf, 2003[75] 2002 Karachi Harm reduction center CS All male, 86% homeless 153 0.0 — Hadi, 2005 [64] 2002 Rawalpindi, Swat, & Mardan Mixed CS 65% male 500 3.4 2.0–5.4 Akhtar, 2004 [186] 2002 Faisalabad Voluntary drug treatment center CS All male 74 0.0 — Nai Zindagi, 1999 [72] 1999 Lahore Community CS All male 200 0.0 — Parviz, 2006 [82] 1996 Karachi Voluntary drug treatment center & community CS All male 231 0.4 0.0–2.4 Baqi, 1998 [81] 1994 Karachi Voluntary and mandatory drug treatment center CS All male 120 0.0 — Iqbal, 1996 [187] 1987–2004 Lahore Clinical setting CS 77 0.0 — Khanani, 2010 [188] — Karachi Clinical setting CS Afghani refugees 42 19.0 8.6–34.1 UrRehman, 2002 [189] — National 400 0.0 — Syria Mental Health Directorate, 2008 [59] 2006 Damascus SBS 96% male 204 0.5 0.1–2.7 Tunisia MOH, 2013 [53] (Round II) 2011 Tunis RDS 506 2.9a 1.3–4.4a Bizerte RDS 301 0.0 — MOH, 2010 [54] (Round I) 2009 Tunis, Bizerte, & Sousse RDS 91% male 715 3.1 1.9–4.6 a Population-adjusted estimate. b Self-report. CS, convenience sampling; ID, infectious disease; MSCS, multi-stage cluster sampling; RCS, random cluster sampling; RDS, respondent driven sampling; SBS, snow ball sampling; SRS, simple random sampling; TLS, time location sampling; VCT, voluntary counseling and testing. Three HIV incidence studies were identified. In Kabul, Afghanistan, HIV incidence among a sample of 479 PWID in 2008 was 2.2/100 person-years (pyr), despite 72% of study participants reporting use of harm reduction services [63]. Among 500 PWID in three cities in Pakistan, HIV incidence was 1.7/100 pyr in 2006 [64]. A very high incidence rate (17.2/100 pyr) was reported in Tehran, Iran, in 2002 among 214 incarcerated PWID [65]. Analysis of notified HIV cases indicated that in 2011, injecting drug use contributed 20% (80/409), 23% (50/216), 38% (6/16), 49% (52/107), and 60% (948/1,588) of all newly notified cases in this year in Egypt, Pakistan, Bahrain, Afghanistan, and Iran, respectively. A smaller contribution was reported in the remaining countries (Table 4). 10.1371/journal.pmed.1001663.t004 Table 4 Contribution of injecting drug use as a mode of HIV transmission to the total HIV/AIDS cases by country as per various studies/reports and countries' case notification reports [126],[190]. Country 2011 Case Notification Reporta Cumulative Data since the Start of the Epidemic n N Percent Percent due to PWID (end year) Afghanistan 52 107 48.6 44.3% (2011) Bahrain 6 16 37.5 62.8% (2008) Egypt 80 409 19.6 1.6% (2008) Iran 948 1,588 59.7 69.4% (2011) Iraq — — — 0.0% (2009) Jordan 0 17 0.0 2.4% (2011) Kuwait 0 25 0.0 2.2% (2008) Lebanon 1 51 2.0 6.1% (2009) Morocco 9 750 1.2 2.7% (2011) Oman 5 140 3.6 4.3% (2011) OPT 0 6 0.0 2.8% (2011) Qatar 0 1 0.0 — Pakistan 50 216 23.1 33.2% (2008) Saudi Arabia 46 394 11.7 6.4% (2009) Syria 0 69 0.0 2.4% (2009) Tunisia 3 73 4.1 24.4% (2009) UAE 1 57 1.8 3.6% (2011) Yemen 1 236 0.4 1.4% (2009) Only the most recent available report was used. a Except for Bahrain, Egypt, and Iraq (2010 report) and Pakistan (2008 report). n, number of positive cases that are PWID; N, total number of positive cases; Percent, percent of positive cases that are PWID out of the total number of positive cases; UAE, United Arab Emirates. HIV Epidemic States The evidence was sufficient to characterize the HIV epidemic state in 13 countries, summarized in Table 5. Details on how the conclusions were reached are in Text S3. 10.1371/journal.pmed.1001663.t005 Table 5 Characterization of the state of the HIV epidemic among people who inject drugs in the Middle East and North Africa based on the HIV biological data and quality and scope of the evidence. Country Level of HIV Prevalence Trend in HIV Prevalence Geographical Distribution Quality and Scope of Evidence Iran Concentrated Established National Conclusive Pakistan Concentrated Emerging National Conclusive Afghanistan Concentrated Emerging At least localized Good Egypt Concentrated Emerging At least localized Good Morocco Concentrated Emerging At least localized Good Libya Concentrated Unknown At least localized Good Bahrain At least outbreak-type — — Limited Oman At least outbreak-type — — Poor Jordan Low-level — — Good Lebanon Low-level — — Good OPT Low-level — — Good Tunisia Low-level — — Good Syria Low-level — — Limited Djibouti Unknown — — Poor Iraq Unknown — — Poor Kuwait Unknown — — Poor Saudi Arabia Unknown — — Poor Sudan Unknown — — Poor Yemen Unknown — — Poor Algeria Unknown — — No evidence Qatar Unknown — — No evidence Somalia Unknown — — No evidence UAE Unknown — — No evidence Countries are sorted by level of HIV prevalence, trend in HIV prevalence, geographical distribution, quality and scope of evidence, then alphabetical order. UAE, United Arab Emirates. Concentrated HIV epidemics Concentrated HIV epidemics among PWID were observed in Iran, Pakistan, Afghanistan, Egypt, Morocco, and Libya (Table 5). Iran is the only country with conclusive evidence for an established concentrated epidemic at the national level. The first HIV outbreaks among PWID in Iran were reported around 1996. HIV prevalence then increased considerably in the early 2000s, reaching a peak by the mid-2000s (Figure 3A). HIV prevalence in the 2006 and 2010 multi-city IBBSS was stable at 15% (n = 2,853 and n = 2,479, respectively) (Figure 4C) [43],[44]. The evidence suggests that the HIV epidemic among PWID in Iran is now established at concentrated levels of about 15%. 10.1371/journal.pmed.1001663.g003 Figure 3 Trend of HIV prevalence among male people who inject drugs in (A) Iran and (B) Pakistan. This graph displays all available HIV prevalence measures for these two countries as extracted from eligible reports (Table 3) and various databases (Table S4). Each dot represents one HIV prevalence measure for the specific year, and the bars around it define the 95% confidence interval. A pattern of established HIV epidemic is observed in Iran (A), while a trend of emerging HIV epidemic is observed in Pakistan (B). 10.1371/journal.pmed.1001663.g004 Figure 4 Trend of HIV prevalence among people who inject drugs, and when available men who have sex with men, in repeated rounds of bio-behavioral surveillance surveys. These graphs display the trend of HIV prevalence in repeated rounds of bio-behavioral surveillance surveys using state of the art sampling techniques for hard-to-reach populations including respondent driven sampling and time-location sampling. Country level and aggregate data of multiple cities/provinces are displayed. For consistency between countries and between different rounds within a given country, unadjusted sample estimates are displayed. Three main patterns of HIV epidemics among PWID are depicted. A pattern of emerging concentrated epidemics is observed in Pakistan (A) and Egypt (B); a pattern of established concentrated epidemic is observed in Iran (B); and a pattern of low-level HIV epidemic is observed in Tunisia (D). In Afghanistan (E), there is an emerging epidemic among PWID in apparently only part of the country; the effect of which was diluted in the second round with the inclusion of new cities with still very limited prevalence. The potential overlap of the HIV epidemics among PWID and MSM is depicted in Pakistan and Egypt. In Pakistan, an emerging HIV epidemic among transgender sex workers is observed, but lags the epidemic among PWID (A). In Egypt, the concentrated epidemic among MSM seems to have preceded the epidemic among PWID (B). In Tunisia, the potential link between the MSM and PWID epidemics is not clear because the studies were conducted after the epidemics had already risen. Emerging concentrated epidemics were seen in Pakistan, Afghanistan, Egypt, and Morocco (Table 5). For example, in Pakistan, after almost two decades of very low HIV prevalence among PWID, a trend of increasing prevalence was observed after 2003 (Figure 3B). This trend is national and ongoing, reaching over 40% in recent studies and with no evidence yet of stabilization (Figure 3B). This trend also manifests itself in the multi-province IBBSS where HIV prevalence among PWID has steadily increased from 10.8% in 2005 (n = 2,431) [52], to 15.8% in 2006 (n = 4,039) [51], 20.8% in 2008 (n = 2,969) [50], and 25.2% in 2011 (n = 4,593) [37] (Figure 4A). In view of the high HIV prevalence, the emerging HIV epidemic in Pakistan is considered advanced. Another example is Egypt where HIV prevalence was also very low for about two decades (Tables 3 and S4), including the first round of IBBSS in 2006 [40],[41], but increased to 6%–7% in both cities surveyed in the most recent IBBSS in 2010 (n = 284 and n = 274) (Figure 4B) [42]. Consistently, 19.6% of the 409 newly notified HIV cases in 2010 in Egypt were due to injecting drug use, compared with only 1.6% of the total notified cases up to 2008 (Table 4). In Afghanistan (Figure 4E) and Morocco, the HIV epidemic among PWID appears to be emerging in at least parts of the country, with notably high HIV prevalence in some settings, but still low HIV prevalence in others (Table 3). The HIV epidemic in Libya is also concentrated, but the trend is unclear. Libya has the highest reported prevalence of HIV among PWID in MENA (87.2%, 95% CI 83.1%–90.6% in the IBBSS in Tripoli [47]). Earlier data, although of unclear quality, also indicate prevalence of up to 59% in 2001 among PWID in Tripoli (Table S4). This indicates a concentrated HIV epidemic among PWID in at least part of Libya. Although the epidemic in Tripoli is most likely to be established, the level of evidence overall is insufficient to characterize whether the national epidemic is emerging, with few outbreaks in the past, or is established with endemic HIV transmission among PWID. “At least outbreak-type” HIV epidemics In Bahrain and Oman, data show that there are, or have been, at least some pockets of HIV infection among PWID, with reported prevalence up to 21.1% (Bahrain, n = 242) [60] and 27% (Oman, n = 33) [58]. However, most available data are from studies with unknown methodology or high ROB; therefore, the quality of evidence is insufficient to indicate whether there is a concentrated epidemic in these two countries, even if localized. Low-level HIV epidemics The HIV epidemic among PWID is low-level in Jordan, Lebanon, Tunisia, OPT, and Syria (Table 5). In these countries (except Syria), at least one round of IBBSS has been conducted, in addition to other data; all indicate limited HIV spread among PWID (Figure 4D; Tables 3 and S4). The contribution of injecting drug use to the total notified cases also remains minimal in these countries, further confirming a low-level epidemic (Table 4). Injecting Risk Behavior Table S5 summarizes injecting risk behavior measures among PWID in MENA. The key risk behavior that exposes PWID to HIV infection is the use of non-sterile injecting equipment. Available data indicate that the lifetime prevalence of sharing needles/syringes among PWID in MENA was as high as 71% [45], 79% [66], 85% [47], 95% [67], and 97% [58] in Jordan, Pakistan, Libya, Iran, and Oman, respectively. The median prevalence of sharing in the last injection was 23% (IQR: 18%–28%). In Pakistan, most injecting occurs in groups and in public places, and reported use of “street doctors” or professional injectors was common, which is associated with high reuse of injecting equipment (Table S5) [50]. In MENA, PWID inject drugs at median of 2.2 injections per day, with reported rates of 3.3 [68] and 5.7 [69] injections per day among some PWID in Iran and Afghanistan, respectively. The median age at first injection was 26 years (IQR: 24–28 years), and the median duration of injecting drugs was 4.6 years (IQR: 3.8–6.1 years) (Table S5). Sexual Risk Behavior The majority of PWID in MENA are sexually active (Table S6). On average, 52% have been ever married (IQR: 35%–56%), 43%–89% report having sex with a regular female partner, 29%–60% reported multiple sexual partnerships, and 18%–42% report sex with non-regular female partners in the last year (Table S6). Reported levels of condom use varied but generally were on the low to intermediate range. Overall, 36% of PWID reported ever using condoms (IQR: 20%–54%) with the lowest prevalence in Afghanistan and Pakistan (10%–38% [70]–[76]), and the highest in Lebanon (88% [77]). Condom use during last sex was reported by 4%–38% of PWID, reaching 66% only in Libya [47]. Only 12%–25% of PWID reported consistent condom use in the last year (Table S6). Mixing with Other High-Risk Populations Risk behaviors of PWID in MENA overlap considerably with other high-risk populations, namely MSM and female sex workers. A median of 18% of male PWID in MENA reported ever having sex with men (IQR: 11%–27%), and a median of 7% did so in the last year (IQR: 2%–10%) (Table S6). The highest rates of same-sex sex have been reported in Pakistan. Reported condom use during anal sex was overall very low (Table S6). PWID in MENA engage in sex work, either through buying or selling sex. A median of 45% reported ever having sex with a sex worker (IQR: 31%–64%), and a median of 23% did so in the last year (IQR: 15%–30%), with generally low levels of condom use (Table S6). Selling sex in the past year was reported by 5%–29% of PWID in Egypt, Iran, Morocco, OPT, and Pakistan (Table S6). Proxy Biological Markers of Risk Behavior There was substantial between-and within-country variation in HCV prevalence among PWID, with a median of 44% (IQR: 31%–64%) (Table 6). Very high HCV prevalence was reported such as in Afghanistan (70%, n = 185, Herat), Egypt (63%, n = 100, Alexandria), Iran (over 80%, n = 386 prisoners, Tehran), Libya (94%, n = 328, Tripoli), Pakistan (94%, n = 161, Karachi), and Saudi Arabia (75%, n = 1,909, Jeddah) (Table 6). These figures are consistent with the reported high levels of sharing of injection equipment, such as in Iran, Pakistan, and Libya (Table S5). 10.1371/journal.pmed.1001663.t006 Table 6 Prevalence of hepatitis C virus among people who inject drugs in the Middle East and North Africa. Country HCV Prevalence Year Sample Size Population Characteristics City Source % 95% CI Afghanistan 70.0 63.1–76.8 2012 185 Predominantly male Herat [39] 57.9 49.8–65.6 2009 159 Predominantly male Herat [38] 49.1 43.7–54.6 2006–2008 340 Predominantly male Herat [127] 37.1 31.5–42.9 2009 286 Predominantly male Kabul [38] 36.6 32.1–41.1 2006–2008 463 Predominantly male Kabul [127] 36.1 31.7–40.5 2007–2009 483 Predominantly male Kabul [69] 27.6 23.1–32.5 2012 369 Predominantly male Kabul [39] 25.5 17.4–35.1 2009 102 Predominantly male Mazar-i-Sharif [38] 25.0 17.3–33.6 2012 117 Predominantly male Charikar [39] 24.1 18.1–30.8 2006–2008 187 Predominantly male Mazar-i-Sharif [127] 18.8 14.3–24.3 2012 254 Predominantly male Mazar-i-Sharif [39] 12.5 6.6–20.8 2006–2008 96 Predominantly male Jalalabad [127] 9.5 5.9–13.8 2012 236 Predominantly male Jalalabad [39] Egypt 63.0 52.8–72.4 1994 100 Alexandria [130] Iran 95.4 77.2–99.9 2002–2003 22 Prisoners Gorgan [160] 88.9 80.0–94.8 2003 81 Predominantly male prisoners Guilian [191] 80.5 76.3–84.4 2001–2002 386 Predominantly male prisoners Tehran [162] 80.1 76.2–83.7 1998 464 Shiraz [168] 80.0 76.0–83.5 2006 454 Predominantly male Tehran [192] 76.8 72.4–80.9 2003 401 Predominantly male prisoners Isfahan, Chaharmahal Bakhtiary, & Lorestan [154] 67.4 49.5–82.6 — 34 Tehran [173] 65.9 59.8–71.7 2008 258 Predominantly male Tehran [140] 64.8 58.4–70.6 2002 249 Prisoners Hormozgan [159] 63.3 56.2–70.0 2005–2007 199 Hamadan [193] 59.4 47.4–68.7 2008 117 Predominantly male Foulad-Shahr [141] 59.4 49.2–69.1 2001–2002 101 Prisoners Mashhad [166] 52.9 35.1–70.2 2007 34 Predominantly male, homeless Tehran [194] 52.1 43.6–60.6 2001–2006 142 Predominantly male Ahfaz [164] 52.0 44.9–59.0 2004 202 Predominantly male Tehran [195] 50.0 11.8–88.2 2008–2009 6 Incarcerated juveniles Isfahan [196] 50.0 21.1–78.9 2006 12 Kermanshah [197] 50.0 41.4–58.6 — 138 Predominantly male Shiraz [170] 47.1 42.8–51.4 2008–2009 531 Predominantly male Isfahan [198] 45.3 40.3–50.3 1995 402 Predominantly male prisoners Tehran [199] 44.4 27.9–61.9 2006–2007 36 Females Tehran [146] 43.4 40.8–45.9 — 1,485 Predominantly male Foulad-Shahr [200] 43.4 40.2–46.6 — 936 Predominantly male National [172] 42.4 — 2009–2010 — Kohgiloyeh & Boyerahmad [201] 42.0 38.8–45.2 — 951 Prisoners Foulad-Shahr [202] 41.6 38.4–44.8 2008–2009 943 Predominantly male prisoners Isfahan [203] 40.3 34.0–46.9 2012–2013 233 Predominantly male Shiraz [134] 38.6 32.1–45.2 2010 226 Predominantly male Tehran, Shiraz, & mashhad [79] 37.5 20.4–54.9 2007–2009 33 Sari [142] 36.6 21.6–52.0 2010 42 Female sexual partners of PWIDs Tehran, Shiraz, & mashhad [79] 36.5 28.2–45.2 2001–2002 132 Predominantly male Tehran [162] 36.0 24.6–48.1 2007 70 Tehran [145] 34.1 30.9–37.4 2006–2007 859 Predominantly male Tehran [146] 34.0 31.8–36.3 2008–2009 1,747 Predominantly male Isfahan [204] 31.5 24.2–39.7 2002 149 Predominantly male prisoners Hamadan [161] 30.9 26.0–36.2 2002–2006 333 Predominantly males, hospitalized for infectious disease Ahfaz [158] 22.8 9.6–41.1 2000–2005 31 Hospitalized for infectious disease Zahedan [167] 16.1 5.5–33.7 2003 31 Rafsanjan [157] 13.0 2.8–33.6 2001–2006 23 Females, hospitalized for infectious disease Kashan [163] 12.9 2.8–33.6 2006 23 Tehran & Hormozgan [56] 11.9 7.5–17.6 2001–2006 177 Predominantly males, hospitalized for infectious disease Kashan [163] 11.3 6.5–17.9 2004 133 Predominantly male Shahr-e-Kord [152] 26.8a 20.9–33.3 2011 209 Predominantly male Tehran [135] Lebanon 51.0 33–74 2007–2008 43 Beirut [46] 5.0 0.6–16.9 2000–2002 40 25% female Beirut [175] Libya 94.2 90.8–96.7 2010 328 Predominantly male Tripoli [47] Morocco 79.2 72.1–85.7 2011–2012 274 Predominantly male Nador [117] 45.6 35.5–56.6 2010–2011 261 Predominantly male Tanger [117] Oman 36.0a 12.8–64.9 — 14 Predominantly male Muscat [58] 11.0a 0.3–48.2 — 9 Predominantly male prisoners Muscat [58] 53.0a 40.0–66.3 — 60 Predominantly male Muscat [58] OPT 40.3 29.2–52.2 2010 192 Predominantly male East Jerusalem [177] Pakistan 94.3 89.7–97.4 2003 161 Karachi [74] 92.9 89.1–95.8 2003 255 Predominantly male Lahore [70] 91.8 88.6–94.4 2004 380 Predominantly male Lahore [205] 89.0 83.8–93.0 1999 200 Predominantly male Lahore [72] 89.0 85.5–91.9 — 400 National [189] 87.0 83.3–90.1 2004 399 Predominantly male Karachi [205] 86.9 80.5–91.8 2002 153 Homeless Karachi [75] 76.0 — 2005 — Predominantly male Lahore [179] 75.0 65.1–83.3 2003 96 Predominantly male Quetta [70] 62.5 24.5–91.5 2007–2009 8 Remote rural population Kech [206] 60.0 45.2–73.6 2004 50 Quetta [181] 46.4 34.5–57.9 — 76 Predominantly male prisoners Kabul [207] 45.2 29.8–61.3 — 42 Afghani refugees Karachi [188] 44.7 39.0–50.5 2003 300 Predominantly male Quetta [184] 42.0 37.6–46.5 2002 500 35% female mix of cities [64] 31.5 25.1–38.4 — 200 Predominantly male Khyber pakhtunkhwa [208] 17.3 13.1–22.0 2007 302 Predominantly male Rawalpindi [178] 14.3 5.4–28.5 — 42 Khyber pakhtunkhwa [209] 8.0 3.4–14.9 2007 102 Predominantly male Abotabad [178] Saudi Arabia 74.6 72.6–76.5 1995–1996 1909 Predominantly male Jeddah [210] 69.0 64.7–72.9 1995–1996 505 [211] 38.1 32.9–43.4 — 344 [212] Syria 60.5 43.4–76.0 2006 38 Predominantly male Damascus [213] 21.0a 11.4–33.9 2006 57 Predominantly male Damascus [59] Tunisia 35.8 29.1–42.5 2011 506 Predominantly male Tunis [53] 29.1 25.8–32.6 2009 701 Predominantly male Tunis, Bizerte, & Sousse [54] 2.4 0.6–4.1 2011 301 Predominantly male Bizerte [53] The table is sorted by country then by descending order of HCV prevalence. a Self report. Available data on the prevalence of syphilis among PWID in Egypt, Iran, Afghanistan, and Pakistan indicate relatively high prevalence up to 3%, 8%, 17%, and 18%, respectively (Table S6). Considerable herpes simplex virus type 2 prevalence has been reported among PWID in Afghanistan (4%–21%) and Pakistan (6%–19%) (Table S6). Data on the prevalence of gonorrhoea (0%–1.8%) and chlamydia (0%–0.7%) were available only in Pakistan (Table S6). Knowledge of HIV/AIDS Levels of basic HIV/AIDS knowledge among PWID in MENA were high overall, with a median of 93% having ever heard of HIV/AIDS (IQR: 72%–99%). Still, there was much variation in the proportion of PWID who correctly identified reuse of non-sterile needles/syringes and unprotected sex as modes of HIV transmission (Table S7). Only a median of 45% (IQR: 30%–63%) of PWID perceived themselves at risk of HIV/AIDS (Table S7). With a few exceptions of high levels of HIV testing such as in Lebanon and Oman, the median prevalence of lifetime testing among PWID ranged between 8% (Egypt) and 45% (Iran) (Table S7). Discussion Injecting Drug Use in MENA We estimate that there are 626,000 PWID in the MENA region. Overall, the mean prevalence of injecting drug use (0.24%) is comparable with global figures which range from 0.06% in South Asia to 1.50% in Eastern Europe [31]. Prevalence of injecting drug use in MENA varied between countries and was higher in the eastern part of the region. Injecting drug use appears to be heavily concentrated among men; but female PWID are one of the hardest-to-reach populations in MENA, thereby limiting our knowledge of this vulnerable group. From limited available data, it appears that injecting drug use among females has a strong association with sex work and having a PWID sexual partner [78],[79]. Emerging HIV Epidemics and HIV Epidemic Potential among PWID After synthesizing a large body of data, we documented HIV epidemics among PWID in one-third of MENA countries. The HIV epidemic is in a concentrated state in about half the countries with available data. Iran is the only country with an established concentrated epidemic, while the most common pattern is that of emerging concentrated epidemics. Most observed epidemics in the region are recent, occurring only in the last decade; around the same time that HIV epidemics among MSM appear to have emerged (2003) [14]. Of note, our classification of epidemic states did not depend only on the size of the epidemic, but also on the trend of HIV prevalence and other biological data. For example in Pakistan, despite high HIV prevalence, the epidemic was classified as emerging since HIV prevalence continues in an increasing trend. HIV prevalence among PWID in MENA countries with concentrated epidemics is overall in the range of 10%–15%, which is in the intermediate range compared to global figures [31]. However, there are settings with very high prevalence, most notably in Tripoli, Libya, which appears to have one of the highest HIV prevalence reported globally (87.1%) [31],[47]. In about 20% of MENA countries, the HIV epidemic among PWID was low level, with HIV prevalence consistently low for many years including the most recent IBBSS. In some countries, such as Jordan, Lebanon, and OPT, no HIV infections were found in the IBBSS. The available evidence in countries at low level is restricted to a few cities, and there could be hidden sub-epidemics in other sites. Nevertheless, the low prevalence could be reflective of the intrinsic HIV transmission dynamics, levels of risk behavior, and/or injecting network structure. HIV may not have been introduced to the PWID community, may have been recently introduced, or may have been spreading slowly and inefficiently for some time. The latter may reflect injecting networks with infrequent and few repeated transmission contacts among PWID to sustain HIV dynamics. In Lebanon and Syria for example, it appears that PWID form closed small networks with injecting occurring in private homes and among friends, and not in large groups or at shooting galleries [59],[80]. The low prevalence could also be a consequence of stochastic effects where the small number of individuals who introduced HIV to the PWID population happened by chance not to have links that could sustain transmission chains. Whilst it is conceivable that HIV prevalence may not grow in countries currently at low level, there are settings where HIV prevalence increased considerably in a short period of time. For example in Karachi, Pakistan, after several years of near zero prevalence [74],[75],[81],[82], HIV prevalence in 2004 increased to 23% in less than 6 months [83], and reached 42% in 2011 [37]. This pattern is not surprising given the reported risky practices and high HCV prevalence. When HIV prevalence was still very low in Karachi, HCV prevalence was over 85% [74],[75], indicating substantial use of non-sterile injecting equipment and suggesting connectivity of injecting networks. In Iran, the substantial HCV prevalence (up to 80%) was predictive of the explosive HIV epidemic that occurred subsequently. In both Iran and Pakistan, injecting networks often seem to be well connected and we found reports of injecting and sharing occurring among persons who are not necessarily socially related, e.g. in shooting galleries [84],[85]. Data on HCV prevalence among PWID in MENA countries with low-level HIV epidemics are limited. However, HCV prevalence of 40%–61% among some PWID groups such as in Lebanon, OPT, and Syria suggest moderate HIV epidemic potential once the virus is introduced to the PWID community. Bridging of the HIV Epidemic to Other Population Groups We found considerable overlap of risk behavior between PWID and other high-risk groups in MENA; this could play a role in emerging HIV epidemics, as it creates opportunities for an infection circulating in one population to be bridged to another one. In Pakistan, the rapidly growing HIV epidemic among PWID was followed closely by an emerging epidemic among transgender sex workers (Figure 4A). Phylogenetic analyses found clustering of subtypes between the two populations, suggesting that the infection might have bridged from PWID to the transgender population [86]. A similar pattern, but in the opposite direction, may have occurred in Egypt where an emerging epidemic among MSM [14] preceded the nascent epidemic among PWID (Figure 4B). While supported by behavioral data [40],[42], this needs to be confirmed by phylogenetic analyses. Our analysis, focused on the HIV disease burden among PWID, still masks the role of these epidemics in driving the onward transmission of HIV to the sexual partners of PWID and further in the population. The majority of PWID are sexually active and about half are married. They often engage in risky sexual behavior as confirmed by the prevalence of STIs. This puts sexual partners of PWID at risk of HIV. A substantial number of infections in MENA have been documented in women who acquired HIV from their PWID husbands; and in some countries, the majority of HIV infections among women were acquired from a PWID sexual partner [79],[87]–[89]. This highlights the vulnerability of sexual partners of PWID, who are often female spouses. An illustration of the role of the HIV epidemics among PWID in driving the onward transmission of HIV emerges from recent mode of transmission (MoT) modeling studies in the region [90]–[92]. For example, in Iran, PWID directly contributed 56% of the total HIV Incidence; and indirectly, only through infections to their current sexual partners, an additional 12% of the total incidence [92]. More onward HIV transmissions would arise if the sexual partners of PWID transmitted the infection to their other sexual partners. Study Limitations One limitation of our study is that the quantity and quality of data varied by countries. There were virtually no HIV data in four countries, and the data quality in six others was insufficient to assess the status of the epidemic. Longitudinal repeated IBBSS data were available in only five countries. Six countries have recently conducted their first round of IBBSS; and in most of these, subsequent rounds are either planned or being implemented. The quality of data was “good” or “conclusive” in ten out of the 23 countries. While most of the data were from cross sectional surveys, there was a substantial improvement in the quality of data over time. Many studies were conducted with state of the art research methodologies in HIV research. These consist of IBBSS studies using innovative sampling methodologies for hard-to-reach populations such as respondent-driven sampling and time-location sampling. Most of these studies benefited from large sample sizes and some from broad geographical coverage at the national level. Of note that in several countries there were no recent national estimates of the number and proportion of PWID. The only national data available for these countries were extracted from earlier global reviews of injecting drug use [4],[31]. The reviews were based mainly on estimates by the Reference Group to the UN on HIV and Injecting Drug Use, which systematically collects and analyses global data on injecting drug use and HIV [32]. The Reference Group is considered the main reference for PWID estimates globally, providing the estimates to the United Nations Office on Drugs and Crime (UNODC), WHO, and UNAIDS secretariats. We complemented the Reference Group data with PWID national risk-group size estimation studies that were conducted in the last few years in five countries namely Afghanistan, Iran, Pakistan, Saudi Arabia, and Tunisia. Since we partly relied on secondary sources of data and since the data that we used came from studies using different methodologies, our pooled estimates of the number and prevalence of PWID in MENA should be considered as approximate figures. In assessing the status of the epidemic at the country-level, we did not limit our analysis to one line of evidence, but synthesized and corroborated findings from different data sources and types such as HIV prevalence and incidence, notified HIV cases, injecting and sexual risk behavior, and other related and contextual data. Thus we could make a comprehensive assessment of the epidemic status and address potential limitations in any one line of evidence [93]. We did a rigorous appraisal of the scope and quality of the evidence within each country by assessing the amount and geographical coverage of available data, as well as the ROB and precision of individual point estimates. A qualifier for the scope and quality of the evidence at the country level was integrated with each HIV epidemic state assigned. Our search criteria were expansive, covering different literature sources. Before the present submitted work, the status of the epidemic across MENA country was poorly understood. On the basis of our integrated data synthesis and using rigorous methodology and data quality assessment, we were able to concretely qualify the epidemic status in 13 countries (over half of MENA countries), and to document the overall trend of emerging epidemics. The lack of evidence in several MENA countries does not preclude the possibility of hidden epidemics among PWID in these settings. HIV Response among PWID in MENA Not only does the region overall lag behind in responding to the emerging HIV epidemics among PWID; in occasions misguided policy has contributed to these epidemics. Most notably in Libya, the large HIV epidemic among PWID appears to have been exacerbated by restrictions imposed on the sale of needles and syringes at pharmacies in the late 1990s [11],[94]. Overall, harm reduction programs still remain limited in MENA, and there is a need to integrate such programs within the socio-cultural framework of the region [95]. Several countries though have made significant strides in initiating such programs in recent years [11],[96]. Needle/syringe exchange programs are currently implemented in nine countries, and opioid substitution therapy in five [96]. Iran remains the leader in the provision of harm reduction services to PWID with the highest coverage of needle/syringe exchange programs in the region [12],[96]. It appears also to be the only country in MENA to provide such services in prisons [96],[97] and to provide female-operated harm reduction services targeted at female drug users [96]. Iran has also initiated triangular clinics that integrate services for treatment and prevention of injecting drug use, HIV/AIDS, and other STIs; and these clinics have received international recognition as best practice [98]–[100]. Among other interventions implemented in Iran are drop-in centers, integration of substance use treatment and HIV prevention into the rural primary health care system, and community education centers [62],[101]–[105]. These efforts appear to have been successful in reducing sharing of injecting equipment [106]–[108], though the coverage of harm reduction continues to be lower than adequate [104]. Other countries in the region have also made progress in revising their policies, adopting harm reduction programs, and integrating such programs in their national strategic plans such as Afghanistan, Egypt, Lebanon, Morocco, Pakistan, and Tunisia [11],[109]. Access to antiretroviral therapy (ART) has also expanded in MENA in recent years, and treatment outcomes reported by country ART programs are comparable to globally reported outcomes [110],[111]. Good adherence to ART has been also observed, such as in Morocco [112], though some non-adherence and treatment interruptions, among other obstacles, have been also reported in several countries [112]–[114]. Non-governmental organizations (NGOs) have been instrumental to the success in harm reduction in MENA. It can be noted that in countries where NGOs are strong, HIV response has been also strong [11],[109]. The Iranian NGO Persepolis, for example, played an important role in the transformation to effective policies in Iran [115]. Building on the growing role of NGOs, a regional civil society network was established in 2007 covering 20 countries in MENA; the Middle East and North Africa Harm Reduction Association (MENAHRA) [116]. MENAHRA has the objective of building the capacity of civil society organizations in harm reduction efforts through training, sharing of information, networking and providing direct support to NGOs to initiate or scale-up harm reduction services. The network is a collaborative initiative by regional and international organizations with funding from international donors, and has been influential in promoting harm reduction. Despite the recent progress in harm reduction, HIV prevention efforts among PWID in MENA remain impeded by generic and routine planning, competing priorities, limited human capital, and lack of monitoring and evaluation [7]. National policies remain inadequate and not sufficiently reflecting evidence-informed approaches [7]. The scope and coverage of prevention services remain patchy across and within countries [11],[96],[109]. An indicator of the low effective coverage is that only a minority of PWID report ever being tested, and a smaller proportion report being tested within the last year [11]. In Morocco and Pakistan, two countries with a strong HIV response, only 32.5% [117], 47.8% [117], 6.1% [51], and 20.7% [50] of PWID in different surveys reported ever being tested. Even where services are available, PWID may not be aware of them, and when aware of them, they may not utilize them. In Pakistan for example, 37% of PWID in one study were aware of HIV prevention programs in their city, but only 19% ever used them [52]. There is an urgent need to expand the provision, scope, and coverage of HIV interventions among PWID in MENA to be ahead of the growing HIV epidemics. Conclusion Our study identified a large volume of HIV-related biological and behavioral data among PWID in the MENA region, including quality data that appear in the scientific literature for the first time. The in-depth analyses, the quality assessment of evidence, and the comprehensive synthesis of data facilitated, for the first time to our knowledge, a rigorous characterization of the state of the epidemic among PWID across different countries in this region. We found robust evidence for HIV epidemics among PWID in multiple countries, most of which have emerged only recently and continue to grow. The high risk and vulnerability context suggest potential for further HIV spread. HIV surveillance among PWID must be expanded to detect and monitor these budding and growing HIV epidemics, and to inform effective HIV policy and programming. This mainly includes conducting IBBSS studies among PWID in countries where such surveys have not been conducted yet, and implementing subsequent rounds, for the provision of longitudinal data, in countries that are already developing their surveillance base. Population size estimations and mapping and ethnographic studies are also needed for a better understanding of the profile and injecting and sexual networks of PWID in MENA. The window of opportunity to control the emerging epidemics should not be missed. HIV prevention among PWID must be made a priority for HIV/AIDS strategies in MENA; and obstacles must be addressed for the provision of comprehensive services and enabling environments for PWID [118]. There is need to review current HIV programs among PWID in light of the emerging epidemics, and to develop service delivery models with embedded links between community-based prevention (needle/syringe exchange programs and condom provision), HIV testing, and treatment (opioid substitution and ART). Such comprehensive approach has already proven its utility in preventing HIV transmission among PWID [119]–[121], but would require better resource allocation and sufficient services in priority areas for PWID. Prevention efforts need to prioritize those most likely to be reluctant to approach facility-based services, and those with multiple and overlapping risks. Outreach and peer education can provide a means to reach those most at risk with information and services. Access to ART should be expanded in such a region with one of the lowest ART coverage globally [122]. Such expansion must address the low diagnosis rate among people living with HIV [110]. Reaching the at-risk populations even in discreet unpublicized ways would contribute positively to HIV prevention [14],[123]. Improving HIV programming among PWID in MENA is essential not only to confront the growing HIV problem in this population group, but also to prevent the onward transmission of HIV, and the bridging of the infection to other groups as has already occurred in parts of the region. Supporting Information Table S1 Precision and risk of bias of individual HIV prevalence measures among people who inject drugs in the Middle East and North Africa as extracted from eligible reports. (DOCX) Click here for additional data file. Table S2 Summary of precision and risk of bias of HIV prevalence measures as extracted from eligible reports. (DOCX) Click here for additional data file. Table S3 Subnational estimates of the number and prevalence of people who inject drugs in the Middle East and North Africa. (DOCX) Click here for additional data file. Table S4 HIV point-prevalence measures among people who inject drugs as extracted from various databases including the US Census Bureau database, the WHO/EMRO testing database, the UNAIDS epidemiological fact sheets databases, and other sources of data with unidentified reports. (DOCX) Click here for additional data file. Table S5 Measures of injecting risk behavior among people who inject drugs in the Middle East and North Africa. (DOCX) Click here for additional data file. Table S6 Measures of sexual risk behavior and sexually transmitted infections prevalence among people who inject drugs in the Middle East and North Africa. (DOCX) Click here for additional data file. Table S7 HIV/AIDS knowledge, perception of risk, and HIV testing among people who inject drugs in the Middle East and North Africa. (DOCX) Click here for additional data file. Text S1 PRISMA checklist. (DOCX) Click here for additional data file. Text S2 Search criteria. (DOCX) Click here for additional data file. Text S3 Narrative justification for quality of the evidence and status of the epidemic at the country level. (DOCX) Click here for additional data file.