- Record: found
- Abstract: found
- Article: found
Poor Recognition of Risk Factors for Hepatitis B by Physicians Prescribing Immunosuppressive Therapy: A Call for Universal Rather than Risk-Based Screening
Read this article at
Abstract
Background
Reactivation of hepatitis B virus (HBV) during immunosuppressive therapy (IST) can lead to severe and even fatal hepatitis but can be largely prevented with prophylactic antiviral therapy. Screening for HBV prior to starting IST is recommended. Both risk-based and universal screening have been recommended by different societies. For effective risk-based screening, physicians must be aware of risk factors for chronic HBV infection.
Methods
The HBV screening practices prior to starting IST of rheumatologists, medical and hematological oncologists were evaluated by survey and chart review. Country of origin, the primary risk factor for HBV exposure, was determined in all patients.
Results
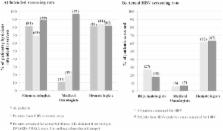
Of 140 rheumatology, 79 medical oncology and 53 hematology patients reviewed, 81%, 11% and 81% were deemed to be at high risk of HBV reactivation by their physicians respectively, however only 27%, 6% and 62% (p<0.0001) were actually screened for HBV prior to starting IST. For patients from HBV-endemic regions, more hematology patients (53%) were correctly identified by their physicians as being at high risk of reactivation than rheumatology patients (2.4%, p=0.0001) or medical oncology patients (15%, p=0.009). However actual screening rates were not increased in patients from endemic regions. A total of 81 patients were screened for HBsAg; 2 were positive. Of the 33 patients screened for anti-HBc, 10 (30%) were positive.
Conclusions
Hematologists, rheumatologists and medical oncologists had low rates of screening for HBV prior to prescribing IST, largely due to poor identification of those at risk for infection. Risk-based screening strategies are unlikely to be effective and should be replaced by universal screening.
Related collections
Most cited references27
- Record: found
- Abstract: not found
- Article: not found
Chronic hepatitis B.
- Record: found
- Abstract: found
- Article: not found