- Record: found
- Abstract: found
- Article: found
Trends in Prevalence and Mortality of Dementia in Elderly Hong Kong Population: Projections, Disease Burden, and Implications for Long-Term Care
Read this article at
Abstract
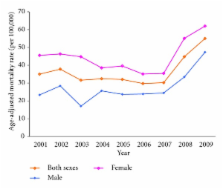
Background. We describe the trends in prevalence and mortality of dementia among older people in Hong Kong over time. Projections of the number of older people with dementia through 2039 and estimation of the disease burden are also included. Methods. Prevalence data were extracted from previous studies in Hong Kong. Mortality data were obtained from the Department of Health of Hong Kong. Projections of the number of people with dementia were calculated by applying the prevalence rates of dementia obtained from previous studies to Hong Kong population projections. The burden of dementia was measured by Disability-Adjusted Life Years (DALYs). Results. The number of people aged 60 and above with dementia is projected to increase by 222%, from 103,433 in 2009 to 332,688 in 2039, with a large proportion of those living in institutions. The number of deaths due to dementia among people aged 60 and above has more than doubled between 2001 and 2009. Mortality rates for dementia have also risen. In 2006, about 286,313 DALYS were lost due to dementia. Conclusions. The information presented may be used to formulate a long-term care strategy for dementia of the ageing population in Hong Kong.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found
Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey
- Record: found
- Abstract: found
- Article: not found