Introduction
Conventional recommendations for diagnostic testing for the evaluation of heart disease in women have largely paralleled those in men. Based on an assumption that stable ischemic heart disease (SIHD) in women was the same as that in men, except occurring about a decade later, traditional efforts focused on the identification of flow-limiting, or obstructive, epicardial coronary artery disease (CAD) as the principal cause of symptoms such as chest pain and dyspnea, common in both women and men. There is now growing recognition that several unique factors related to the presentation, diagnosis, and underlying pathophysiology of SIHD in women necessitate a more rigorous and evidence-based approach to the assessment of their risk, complete with guidelines for sex-specific management strategies when appropriate [1, 2]. Still, because most recommendations have derived predominantly from studies performed in men, the diagnostic utility and accuracy of testing in women has been limited at times by discrepancies between predicted and actual probabilities of obstructive CAD in these patients. Currently, few high-quality data exist regarding optimal diagnostic strategies for the assessment of symptomatic women to establish or exclude a diagnosis of SIHD.
Despite this, heart disease remains the leading cause of death in women worldwide [3], and important sex differences in the rates of diagnosis, utilization of care, response to therapy, and clinical outcomes have been described [4, 5, 6, 7]. Although these partly reflect that women outnumber men in elderly populations at greatest risk of heart disease, women often present with a higher burden of comorbidities and experience worse outcomes than men. Women relative to men have a higher prevalence of persistent angina, nonobstructive CAD, coronary microvascular dysfunction (CMD), spontaneous coronary artery dissection, stress-induced cardiomyopathy, and heart failure with preserved ejection fraction (HFpEF) [8, 9, 10, 11, 12, 13, 14, 15, 16]. Cardiovascular risk factors, including diabetes mellitus [17] and atrial fibrillation [18], are associated with higher rates of vascular complications in women versus men, and women account for a disproportionate burden of inflammatory diseases such as rheumatoid arthritis, which have also been linked to increased cardiovascular morbidity [19, 20]. Women presenting with acute coronary syndromes experience higher mortality than men [21, 22, 23, 24], with lower use of cardiac device therapy [25, 26, 27] despite data showing increased benefit [28], and are referred for cardiac transplantation at later stages of heart failure [29].
As a result of a greater symptom burden and rate of functional disability in women, together with a lower prevalence of obstructive CAD as determined by coronary angiography, the evaluation of SIHD in women as compared with men can present unique challenges to clinicians. The accuracy of standard noninvasive diagnostic testing for ischemia, such as stress testing with exercise electrocardiography, echocardiography, or semiquantitative nuclear myocardial perfusion imaging, can differ significantly when evaluated against a gold standard of identifying anatomically obstructive CAD. This is an especially important consideration for women, whose symptoms are less likely to be explained by findings on coronary angiography and whose abnormal stress test results in the absence of obstructive CAD are more likely to be interpreted as “false positives” [1, 2]. Despite this, women with angina and confirmed ischemia have increased mortality associated with heart disease [30]. This overview highlights how the recent application of novel noninvasive clinical diagnostic tools, including cardiac computed tomography angiography (CCTA), positron emission tomography (PET), and cardiac magnetic resonance (CMR) imaging, is leading to a paradigm change in how heart disease is diagnosed [31, 32] by broadening the definitions of CAD and ischemia, respectively, to better reflect pathological phenotypes more prevalent in women.
Moving Beyond Diagnosis of Obstructive Coronary Artery Disease
Obstructive CAD, defined anatomically on coronary angiography as luminal narrowing of 70% or greater in the major epicardial arteries (or 50% or greater in the left main artery), is neither necessary nor sufficient to explain symptoms of SIHD [33, 34]. Indeed, women present more frequently than men with symptoms of angina [9], but are less likely to manifest obstructive CAD. In a contemporary cohort of 11,223 symptomatic patients (42% women) referred for nonurgent coronary angiography, one-third of men but two-thirds of women had no obstructive CAD, and these patients still experienced an elevated risk of major adverse cardiovascular events (MACEs) [10] (Figure 1). Among patients with stable angina who are found to have obstructive CAD, sex differences also exist in the extent and severity of disease, with women less likely than men to have obstructive multivessel disease [35, 36]. Sex differences in angiographic findings have been demonstrated not only in SIHD patients but also in patients presenting with acute coronary syndromes, including unstable angina and myocardial infarction [37, 38, 39]. In autopsy evaluations of patients who died of ischemic heart disease, women demonstrated less extensive and less obstructive CAD than men, despite pathological evidence of myocardial infarction [40], with more evidence of plaque erosion than plaque rupture [41]. Despite consistently documented lower angiographic disease burden and more often preserved left ventricular function in women with ischemic heart disease, women and men have similar adverse outcomes [42, 43].

Degree of coronary artery disease (CAD) by sex and year of invasive coronary angiography examination.
Reproduced with permission from [10].
This paradox may be at least partly explained by the finding that a visually normal coronary angiogram does not necessarily indicate a normal coronary circulation. Beyond obstructive CAD, vascular dysfunction in the form of abnormal coronary reactivity often coexists with diffuse, nonobstructive atherosclerotic plaques and CMD [12, 36, 44, 45]. Although invasive coronary angiography using visual assessments of epicardial coronary luminal patency remains a cornerstone of cardiovascular disease diagnosis, it has limited ability to identify diffuse atherosclerosis and small-vessel dysfunction (Figure 2). The addition of the use of invasive fractional flow reserve, an assessment of the pressure drop across a focal epicardial stenosis, to coronary angiography has proven beneficial to identify lesion-specific ischemia and guide revascularization [46], but may still underestimate the integrated contribution of diffuse atherosclerosis and small-vessel disease to myocardial ischemia [47, 48]. Nonobstructive CAD and CMD have been implicated in adverse cardiovascular outcomes, including acute coronary syndromes, heart failure and death from plaque erosion, and impaired vasoreactivity with ensuing myocardial ischemia [37, 39, 40, 41]. As a result, testing for SIHD, especially in women, is now moving beyond testing for the presence or absence of obstructive epicardial CAD, which is only one of several possible contributors to myocardial ischemia. Over the last decade, the clinical integration of advanced diagnostic imaging tools is helping to redefine ischemic heart disease and highlight the importance of nonobstructive CAD and CMD. Specifically, noninvasive approaches using CCTA, PET, and CMRI have provided very sensitive assessments for the evaluation of anatomic atherosclerotic plaque, functional ischemia, and myocardial fibrosis, respectively.
Detection of Atherosclerotic Plaque and Nonobstructive Coronary Artery Disease
Noninvasive CCTA has dramatically increased test sensitivity for the diagnosis of CAD and also enabled early characterization of plaque morphology. Recent observational studies have revealed stepwise incremental risk of adverse events in patients along a continuum of both severity (i.e., mild, moderate, or severe stenosis) and extent (i.e., number of involved segments or vessels) of atherosclerotic plaque [10, 49, 50, 51]. Accelerated by the growth of CCTA, mounting evidence now supports that (1) the presence of any atherosclerotic plaque, obstructive or not, portends increased risk of events and (2) the higher the overall plaque burden that is present, the higher the risk. From the Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry (CONFIRM), in which 23,854 consecutive patients without known CAD (33% asymptomatic) underwent CCTA between 2005 and 2009, per-patient nonobstructive and obstructive CAD conferred increased risk of death in a stepwise manner as compared with absence of CAD, which was associated with very low risk [51]. In a subsequent sex-specific subgroup analysis of patients with no or nonobstructive CAD (n=18,158), nonobstructive CAD was associated with a modest adjusted risk of MACEs (composite of death and nonfatal myocardial infarction) that was similarly increased in both women and men [52]. Also, in a smaller subset of patients with longer follow-up (n=5632 followed up for 5 years, 30% with nonobstructive CAD), there was no effect of sex on the association between per-vessel extent of obstructive CAD and MACEs (Figure 3), and the study authors concluded that exploratory analyses of atherosclerotic burden did not identify sex-specific patterns predictive of MACEs [53]. Thus, women and men with comparable risk and extent of CAD had comparable prognosis. Nonetheless, prevalent patterns of disease do differ between women and men, with more symptomatic women than symptomatic men manifesting nonobstructive CAD rather than obstructive CAD [10, 36, 42], with important implications for diagnosis and management.

Unadjusted rate of major adverse cardiovascular events (death or myocardial infarction) by sex and coronary artery disease (CAD) extent in a subset of patients from the Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry (CONFIRM) followed up for 5 years.
Increased per-vessel CAD extent was associated with a greater number of major adverse cardiovascular events over time in both (A) women and (B) men (P<0.001 by log-rank test for both). LM, left main coronary artery; 1VD one-vessel disease; 2VD, two-vessel disease; 3VD, three-vessel disease. Reproduced with permission from [53].
Among nonobstructive plaques, CCTA also allows characterization of high-risk plaque features, including positive remodeling, low CT attenuation, or napkin-ring sign consisting of ringlike peripheral higher CT attenuation with central low attenuation. In an observational substudy [54] of the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) including 4415 symptomatic outpatients (52% women) who underwent CCTA and were followed up for a median of 25 months for a composite of MACEs (death, myocardial infarction, and hospitalization for unstable angina), the presence of high-risk plaque in patients with nonobstructive CAD increased the adjusted risk of adverse events 1.6-fold, and high-risk plaque was more strongly associated with events in women (adjusted hazard ratio 2.41, 95% confidence interval 1.25–4.64) than in men (adjusted hazard ratio 1.40, 95% confidence interval 0.81–2.39). Nonetheless, the positive predictive value for MACEs of high-risk plaque detection in these patients was low (only 4.8% of patients with high-risk plaque experienced MACEs), limiting its current clinical applicability.
Diagnosing Coronary Microvascular Ischemia and Dysfunction
Neither conventional angiography nor CCTA can detect CMD, which is defined not anatomically but functionally as a reduced coronary flow reserve (CFR) in the absence of flow-limiting CAD [45]. Global CFR, calculated as the ratio of hyperemic to rest absolute myocardial blood flow averaged over the left ventricle, is an integrated marker of coronary vasomotor dysfunction that measures the hemodynamic effects of focal, diffuse, and small-vessel CAD on myocardial tissue perfusion [55, 56], and has emerged as an important prognostic imaging marker of cardiovascular risk. Observational data have shown that CFR measurements obtained with cardiac PET distinguish patients at low or high risk of MACEs, including cardiac death [57, 58, 59, 60], beyond comprehensive clinical assessment, myocardial perfusion defects, left ventricular ejection fraction (LVEF), low-level troponin elevation [61], diastolic dysfunction [62], or plaque severity on invasive coronary angiography [63]. In parallel to findings with atherosclerotic plaque, evidence now supports that (1) the existence of impaired CFR, whether in the presence or in the absence of obstructive CAD, portends increased risk of cardiovascular events and (2) the more severely impaired the overall global CFR, the higher the risk. Whereas CFR of 2 or greater in patients without severe myocardial perfusion defects effectively excluded high-risk angiographic CAD and was associated with low rates of annualized cardiac death [64], event rates for those with CFR less than 2 increased exponentially as CFR decreased [59, 65, 66]. Because CFR is a measure of not only the effects of epicardial obstructive CAD but also of the effects diffuse atherosclerosis and CMD on myocardial tissue perfusion, worse prognosis in patients with CFR less than 2 may be related to coronary vasomotor dysfunction arising from a mix of pathophysiologic CAD phenotypes. As such, it may be particularly useful for diagnosis and prognosis of symptomatic women with suspected SIHD.
CMD often coexists with diffuse, nonobstructive atherosclerosis [44, 45, 63]. Similarly to CCTA findings for nonobstructive CAD, cardiac PET studies support that CMD is prevalent in symptomatic patients, affecting approximately 50% of patients who were found to have normal myocardial perfusion imaging and LVEF following referral for noninvasive evaluation (Figure 4A) [11]. When present, CMD was associated with adverse cardiovascular events independently of sex (Figure 4B), but was more common in women, who accounted for two-thirds of these patients. Although most patients had some atherosclerotic plaque, the results were consistent even in patients with a coronary artery calcium (CAC) score of 0, and global CFR, but not CAC score, provided significant incremental risk stratification over clinical risk score for prediction of MACEs. Thus, symptomatic patients who do not demonstrate regional ischemia associated with flow-limiting CAD may have diffuse atherosclerosis and CMD for which a more sensitive, quantitative assessment of ischemia may better diagnose abnormalities and identify novel targets for systemic therapies. Although not a uniquely female disorder, this pattern of abnormalities may be more prognostically useful in women. Smaller epicardial coronary arteries in women [67, 68, 69] coupled with differences in shear stress [70] and inflammatory mediators over the lifespan may modify the development of CAD into a diffuse pattern with more contribution from CMD than focal obstruction. Such an effect would be consistent with previously described clinical and pathological observations of sex differences in the presentation of SIHD.

(A) Prevalence of coronary microvascular dysfunction, defined by coronary flow reserve (CFR) less than 2, in symptomatic women and men referred for cardiac positron emission tomography/computed tomography with normal myocardial perfusion. (B) Adjusted cumulative rate of major adverse cardiovascular events by sex and CFR in patients with normal myocardial perfusion. Adapted with permission from [11].
There is emerging evidence that women with very low CFR may be at an especially elevated risk of adverse cardiovascular events (Figure 5A). In symptomatic patients referred for invasive coronary angiography after cardiac PET, women had a lower pretest probability of CAD and a lower burden of obstructive CAD relative to men, but were not protected from MACEs [36], consistent with previously described epidemiologic trends. Although outcomes for men were closely associated with the presence or absence of severely obstructive CAD, in women only those with impaired CFR demonstrated a significantly increased adjusted risk of MACEs. The excess cardiovascular risk observed in women relative to men referred for coronary angiography was independently associated with and mediated by impaired CFR, not obstructive CAD (P for interaction 0.04). Whereas most men with severely impaired CFR were found to have one-vessel, two-vessel, or three-vessel CAD on coronary angiography, most women with similarly impaired CFR demonstrated nonobstructive or one-vessel CAD (Figure 5B). In adjusted analysis, approximately 40% of this observed differential effect of sex on outcomes was mediated by CFR [36].

(A) Log adjusted hazard for major adverse cardiovascular events by sex and coronary flow reserve (CFR). (B) Patients with severely impaired CFR (<1.6) by angiographic disease and sex categories. CAD, coronary artery disease; LAD, left anterior descending artery; LM, left main artery; 1VD, one-vessel disease; 2VD, two-vessel disease; 3VD, three-vessel disease. Adapted with permission from [36].
A very low CFR may represent a critical link to understanding the hidden biological risk of SIHD among women. When present, this abnormality is associated with increased cardiovascular risk in both women and men, but may constitute an especially malignant phenotype in a subset of severely affected women [36], with important implications for their treatment. Data [63] support that revascularization, especially by coronary arterial bypass grafting, in individuals with severely impaired CFR may be beneficial. That the effects of sex differences on outcomes of cardiovascular events are amplified in those with severely impaired CFR further suggests that certain patients (e.g., with very low CFR and less obstructive CAD, a phenotype more prevalent in women and less amenable to focal revascularization) may be at especially high risk (Figure 6) [36]. Instead of being interpreted as demonstrating a “false positive” (or in some cases negative) traditional ischemic evaluation, patients with impaired CFR and less obstructive CAD may be at significantly increased CVD risk despite having access to revascularization, which is fundamentally targeted at management of obstructive CAD. Thus, although providing optimal, equitable guideline-directed care remains a critical goal for treating women with SIHD, doing so according to current paradigms may be insufficient to address what is likely a combination of biological and environmental determinants of their prognosis. Additional research is needed to determine precisely what is optimal care for this subset of vulnerable patients (Figure 7). These findings may be especially relevant in women with risk factors including obesity [71], diabetes, and/or metabolic syndrome, and autoimmune inflammatory disease, as well as those with HFpEF and ischemia with no obstructive CAD (INOCA) [72].

Model of prevalent pathological phenotypes in women and men with ischemic heart disease with possible impact on cardiovascular management strategies and outcomes.
CABG, coronary artery bypass graft; CFR, coronary flow reserve; CVD, cardiovascular disease; GDMT, guideline-directed medical therapy; HFpEF, heart failure with preserved ejection fraction; MBF, myocardial blood flow; PCI, percutaneous coronary intervention; 1 VD, one-vessel disease. Reproduced with permission from [36].
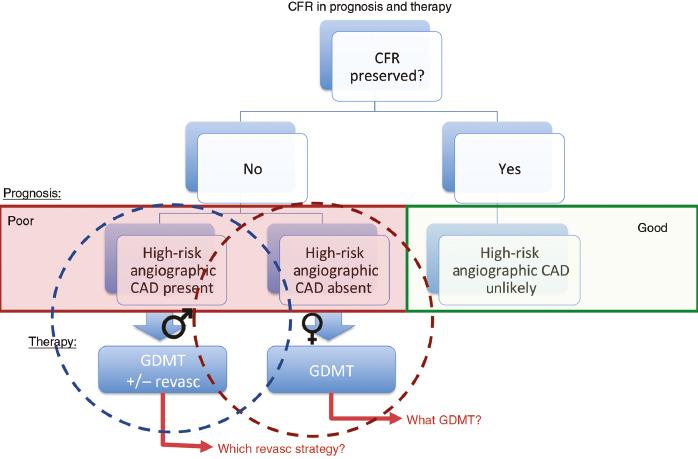
Conceptual summary of coronary flow reserve (CFR) in prognosis of and therapy for patients with suspected ischemic heart disease.
High-quality prospective trials are needed to evaluate the role of CFR as a useful biomarker for patient selection in assessments of ischemia-driven revascularization and for investigations of the effects of novel systemic therapies on cardiovascular outcomes, particularly in specific subsets of vulnerable patients such as women. CAD, coronary artery disease; GDMT, guideline-directed medical therapy; Revasc, revascularization. Adapted with permission from [66].
Identification of Subclinical Myocardial Scar
In addition to cardiac PET, CMR has been used to evaluate selected patients for CMD [73, 74]. Its unique strength lies in its superior spatial resolution, allowing the comprehensive assessment of cardiovascular structure and function, including the sensitive quantification of myocardial scar. In myocardial infarction, necrotic myocardium undergoes replacement fibrosis in which collagen fiber deposition results in expansion of the extracellular space. CMR techniques can be used to evaluate focal changes at the tissue level, including edema, microvascular obstruction, and the progression of replacement fibrosis to fully developed regional scar using late gadolinium enhancement (LGE) [75]. Gadolinium, an extracellular contrast agent, demonstrates slow washout from areas of fibrosis relative to normal myocardium, which allows visualization of subcentimeter lesions on delayed images on CMR, with distinction between subendocardium, midmyocardium, and subepicardium involvement. Among symptomatic women (n=341) with suspected ischemia but no obstructive CAD and preserved LVEF who underwent LGE CMR in the Women’s Ischemia Syndrome Evaluation–Coronary Vascular Dysfunction (WISE-CVD) study, the prevalence of LGE was 8%, and one-third of affected women did not have a prior diagnosis of myocardial infarction despite most patients demonstrating a scar pattern typical of CAD [76]. An emerging technique for assessment of tissue remodeling by CMR involves T1 mapping with and without gadolinium to measure the extracellular volume fraction and native myocardial T1, respectively. Extracellular volume fraction has been correlated with diastolic dysfunction in HFpEF patients [77] and may be a biomarker of diffuse myocardial fibrosis. Native T1 mapping has recently been proposed for diagnosis of myocardial ischemia with and without obstructive CAD [78]. In a recent pilot study involving participants in the WISE-CVD study, native T1 was significantly increased in symptomatic INOCA patients relative to controls, and was associated with reduced myocardial perfusion reserve index [79].
Putting It All Together: Patient Selection for Testing
The role of any imaging procedure, in women or men, is to provide information that refines the clinician’s decision-making process with the goal of relieving patient symptoms and bettering clinical outcomes. In the setting of chest pain or ischemic equivalent symptoms, the prevalence of CAD differs depending on patient characteristics, including not only sex but also age, coronary risk factors, and the nature of the presenting symptoms. Low-risk individuals are unlikely to benefit from the addition of imaging for the purposes of CAD diagnosis or risk stratification regardless of the imaging modality used [1, 80, 81]. This concept was illustrated in PROMISE, which randomized 10,003 symptomatic patients to a strategy of initial anatomic testing (using CCTA) or functional testing (using exercise electrocardiography, nuclear stress testing, or stress echocardiography) [82]. Although the approximately 3% event rate over a median of approximately 2 years of follow-up was lower than predicted by the study investigators, this finding is less surprising when one considers that 78% of enrolled patients with angina had atypical symptoms, and in the CCTA arm, more than one-third of patients demonstrated a CAC score of 0 [83]. This has led some to question not whether an anatomic versus functional strategy was superior but whether any testing versus a deferred testing strategy would have been appropriate. Indeed, over the last two decades, we have witnessed falling diagnostic yields for noninvasive stress testing [84] and invasive coronary angiography [10, 85], reflecting the referral of patients with lower risk and less prevalent obstructive CAD.
This phenomenon has been particularly problematic for women, for whom continued use of traditional risk tables based on decades-old approaches to estimate the pretest probability of obstructive CAD has led to systematic overestimation of risk [86]. However, although an initial testing strategy is not recommended in low-risk women with stable chest pain, it has become unclear how to best define who is at low risk. The 2016 guidelines from the UK National Institute for Health and Care Excellence (NICE) [87], which favor first-line use of CCTA for the evaluation of patients with new-onset chest pain due to suspected CAD, have led to controversy about whether assessment of patient pretest probability remains a sound clinical strategy. In considering this question, however, one must recognize two major issues. The first is that the updated NICE recommendations apply only to patients without known CAD who present with certain characteristic anginal symptoms and a normal ECG, all of which does, in effect, still require consideration of a patient’s likelihood of having disease, and which still depends on accurate classification of sometimes vague symptoms. Secondly, in determining the accuracy of risk assessments, one must also consider pretest risk of what exactly? As already discussed, a symptomatic patient’s risk of obstructive CAD versus flow-limiting CAD versus microvascular ischemia and CMD may be very different and cannot be assessed with a one-size-fits-all approach. Although many low-risk women may benefit from a deferred testing or no imaging strategy, some women may require additional specialized testing with advanced imaging techniques (Figure 8).

Proposed clinical algorithm for the preferred initial diagnostic evaluation of symptomatic women with suspected stable ischemic heart disease with or without obstructive coronary artery disease (CAD).
The algorithm assumes the test is locally available and as low as reasonably achievable (ALARA) principles for radiation dose reduction strategies (i.e., prospective ECG-gated computed tomography [CT], avoidance of dual-isotope and 201Tl single-photon emission CT [SPECT] protocols, and preference for cadmium zinc telluride and stress-only SPECT, or positron emission tomography [PET]) are used whenever possible. In cases where an anatomic strategy (i.e., cardiac CT angiography [CCTA] or invasive coronary angiography) demonstrates absence of obstructive CAD, one should consider PET coronary flow reserve [CFR] evaluation for coronary microvascular dysfunction. If nonobstructive CAD and/or coronary microvascular dysfunction is present, the patient should be referred for guideline-directed therapies (where paucity of data and guidelines suggests more research is needed to define optimal therapies). ETT, exercise treadmill testing; MPI, myocardial perfusion imaging. Reproduced with permission from [2].
The limited accuracy of conventional stress testing for the diagnosis of CMD and its increased prevalence in women underscore the importance and complementary value of assessing both the macrocirculation and the microcirculation in symptomatic women with suspected SIHD. In women with refractory angina, CMD may be the culprit. Identification of no CAD or nonobstructive CAD in these patients, particularly in the setting of documented ischemia, should trigger consideration of CMD, with referral for specialized testing, such as with PET, to interrogate coronary microvascular function [72, 88]. In the future, additional assessments of atherosclerotic plaque burden and diffuse myocardial fibrosis using CCTA and CMRI, respectively, may also further refine risk assessment and help focus management strategies in affected women (Figure 9).

Top priorities for cardiovascular (CV) imaging in women.
Reproduced with permission from [2].
Conclusion
The evaluation of SIHD in women as compared with men can present unique challenges to clinicians. Designed primarily for the identification of obstructive CAD, traditional diagnostic testing approaches for suspected SIHD can lead to overtesting in women without differentiating who is truly at risk. Moving forward, our collective goal must emphasize how to identify women at high risk of adverse cardiovascular events (not anatomically obstructive CAD per se) without overtesting those at low risk. More recently, the clinical integration of advanced diagnostic imaging tools such as CCTA, PET, and CMR is enabling very sensitive assessments of anatomic atherosclerotic plaque burden, macrovessel- and microvessel-related ischemia, and myocardial fibrosis, respectively. Application of these novel technologies promises to broaden definitions of CAD and ischemia to better reflect the whole spectrum of pathological phenotypes in women, including nonobstructive CAD and CMD, and aid in the development of innovative and evidence-based strategies for their management.

