- Record: found
- Abstract: found
- Article: found
PrePex Male Circumcision: Follow-Up and Outcomes during the First Two Years of Implementation at the Rwanda Military Hospital.
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
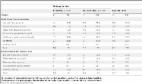
PrePex Male Circumcision (MC) has been demonstrated as an effective and scalable strategy to prevent HIV infection in low- and middle-income countries. This study describes the follow-up and outcomes of clients who underwent PrePex MC between January 2011 and December 2012 with weekly follow-up at the Rwanda Military Hospital, the first national hospital in Rwanda to adopt PrePex.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Male circumcision for HIV prevention in sub-Saharan Africa: who, what and when?
Anne Buvé, David J G White, Judith R Glynn … (2008)
- Record: found
- Abstract: found
- Article: not found
HIV prevention: male circumcision comparison between a nonsurgical device to a surgical technique in resource-limited settings: a prospective, randomized, nonmasked trial.
Jean Bitega, S. Kaplan, E Rwamasirabo … (2012)
- Record: found
- Abstract: found
- Article: found
Safety, Effectiveness and Acceptability of the PrePex Device for Adult Male Circumcision in Kenya
Paul J. Feldblum, Elijah Odoyo-June, Walter Obiero … (2014)