- Record: found
- Abstract: found
- Article: found
Financial barriers and adverse clinical outcomes among patients with cardiovascular-related chronic diseases: a cohort study
Read this article at
Abstract
Background
Some patients with cardiovascular-related chronic diseases such as diabetes and heart disease report financial barriers to achieving optimal health. Previous surveys report that the perception of having a financial barrier is associated with self-reported adverse clinical outcomes. We sought to confirm these findings using linked survey and administrative data to determine, among patients with cardiovascular-related chronic diseases, if there is an association between perceived financial barriers and the outcomes of: (1) disease-related hospitalizations, (2) all-cause mortality and (3) inpatient healthcare costs.
Methods
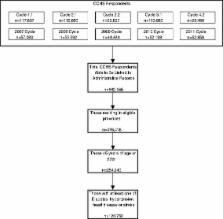
We used ten cycles of the nationally representative Canadian Community Health Survey (administered between 2000 and 2011) to identify a cohort of adults aged 45 and older with hypertension, diabetes, heart disease or stroke. Perceived financial barriers to various aspects of chronic disease care and self-management were identified (including medications, healthful food and home care) from the survey questions, using similar questions to those used in previous studies. The cohort was linked to administrative data sources for outcome ascertainment (Discharge Abstract Database, Canadian Mortality Database, Patient Cost Estimator). We utilized Poisson regression techniques, adjusting for potential confounding variables (age, sex, education, multimorbidity, smoking status), to assess for associations between perceived financial barriers and disease-related hospitalization and all-cause mortality. We used gross costing methodology and a variety of modelling approaches to assess the impact of financial barriers on hospital costs.
Results
We identified a cohort of 120,752 individuals over the age of 45 years with one or more of the following: hypertension, diabetes, heart disease or stroke. One in ten experienced financial barriers to at least one aspect of their care, with the two most common being financial barriers to accessing medications and healthful food. Even after adjustment, those with at least one financial barrier had an increased rate of disease-related hospitalization and mortality compared to those without financial barriers with adjusted incidence rate ratios of 1.36 (95% CI: 1.29–1.44) and 1.24 (1.16–1.32), respectively. Furthermore, having a financial barrier to care was associated with 30% higher inpatient costs compared to those without financial barriers.
Discussion
This study, using novel linked national survey and administrative data, demonstrates that chronic disease patients with perceived financial barriers have worse outcomes and higher resource utilization, corroborating the findings from prior self-report studies. The overall exposure remained associated with the primary outcome even in spite of adjustment for income. This suggests that a patient’s perception of a financial barrier might be used in clinical and research settings as an additional measure along with standard measures of socioeconomic status (ie. income, education, social status).
Conclusions
After adjusting for relevant covariates, perceiving a financial barrier was associated with increased rates of hospitalization and mortality and higher hospital costs compared to those without financial barriers. The demonstrable association with adverse outcomes and increased costs seen in this study may provide an impetus for policymakers to seek to invest in interventions which minimize the impact of financial barriers.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Full coverage for preventive medications after myocardial infarction.
- Record: found
- Abstract: found
- Article: not found
The role of patient navigators in eliminating health disparities.
- Record: found
- Abstract: found
- Article: not found