- Record: found
- Abstract: found
- Article: found
Recurrent Carotid Cavernous Fistula Originating from a Giant Cerebral Aneurysm after Placement of a Covered Stent
Read this article at
Abstract
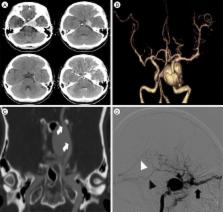
We report the case of a recurrent carotid cavernous fistula (CCF) originating from a giant cerebral aneurysm (GCA) after placement of a covered stent. A 47-year-old woman presented with sudden onset of severe headache, and left-sided exophthalmos and ptosis. Cerebral angiography revealed a CCF caused by rupture of a GCA in the cavernous segment of the left internal carotid artery. Two covered stents were placed at the neck of the aneurysm. The neurological symptoms improved at first, but were aggravated in the 6 months following the treatment. Contrast agent endoleak was seen in the distal area of the stent. Even though additional treatments were attempted via an endovascular approach, the CCF could not be cured. However, after trapping the aneurysm using coils and performing superficial temporal artery-middle cerebral artery bypass, the neurological symptoms improved. In cases of recurrent CCF originating from a GCA after placement of a covered stent, it is possible to treat the CCF by endovascular trapping and surgical bypass.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate.
- Record: found
- Abstract: found
- Article: not found
Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons.
- Record: found
- Abstract: found
- Article: not found