- Record: found
- Abstract: found
- Article: found
Myocardial Ischemia Caused by Paroxysmal Supraventricular Tachycardia in a Patient with Anomalous Origin of Right Coronary Artery Arising from Left Sinus of Valsalva
Read this article at
Abstract
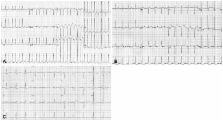
Anomalous origin of a coronary artery is rare and does not generally lead to myocardial infarction and paroxysmal supraventricular tachycardia (PSVT). We report an uncommon case of anomalous origin of the right coronary artery (RCA) originating from the left sinus of Valsalva with PSVT and myocardial ischemia. A 58-year-old man presented with PSVT. After arrhythmia subsided, electrocardiogram showed ST and T wave abnormalities, and transient cardiac enzymes were found to be elevated. Coronary CT angiography confirmed that there was anomalous origin of the RCA originating from the left sinus of Valsalva and no intracoronary stenotic lesion. He was managed with conservative treatment, having no symptoms on clinical follow-up for 4 years.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Coronary artery anomalies in 126,595 patients undergoing coronary arteriography.
- Record: found
- Abstract: not found
- Article: not found
Coronary anomalies: incidence, pathophysiology, and clinical relevance.
- Record: found
- Abstract: found
- Article: not found