- Record: found
- Abstract: found
- Article: found
Comparison of Devices Used for Stent-Assisted Coiling of Intracranial Aneurysms
Read this article at
Abstract
Introduction
Two self-expandable stents, the Neuroform and the Enterprise stent, are widely used for stent-assisted coiling (SAC) of complex shaped intracranial aneurysms. However, comparative knowledge about technical feasibility, peri- and post-procedural morbidity and mortality, packing densities as well as follow-up data is limited.
Material and Methods
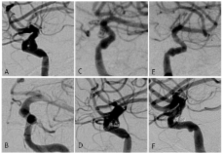
We conducted a retrospective study to investigate differences in aneurysms stented with the Enterprise or Neuroform stents. Angiographic follow-up (mean 19.42 months) was available in 72.6% (61/84) of aneurysms treated with stent-assisted coiling. We further sought to compare stent-assisted coiling to a matched patient population with aneurysms treated by conventional coil embolization.
Results
The stenting success rate of the Enterprise was higher compared to the Neuroform stent (46/48 and 42/51, respectively). In 5 of 9 cases in which the Neuroform stent was not navigable to the landing zone, we successfully deployed an Enterprise stent instead. Eventually, 42 aneurysms were coiled after stenting in each group. We observed no significant differences in peri-procedural complication rate, post-procedural hospital stay, packing density, recurrence rate or number of in-stent stenosis. Strikingly, 36.1% of followed aneurysms in the SAC group showed progressive occlusion on angiographic follow-up imaging. The packing density was significantly higher in aneurysms treated by SAC as compared to conventionally coiled aneurysms, while recanalization rate was significantly lower in the SAC group.
Conclusion
The procedural success rate is higher using the Enterprise, but otherwise both stents exhibited similar characteristics. Lower recurrence frequency and complication rates comparable to conventional coil embolization emphasize the importance of stent-assisted coiling in the treatment of complex aneurysms. Progressive occlusion on angiographic follow-up was a distinct and frequent observation in the SAC group and may in part be due to flow diversion.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms.
- Record: found
- Abstract: found
- Article: not found
Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT).
- Record: found
- Abstract: found
- Article: not found