- Record: found
- Abstract: found
- Article: found
Assessment of Vascular Event Prevention and Cognitive Function Among Older Adults With Preexisting Vascular Disease or Diabetes : A Secondary Analysis of 3 Randomized Clinical Trials
Read this article at
Key Points
Findings
In this secondary analysis of 3 randomized clinical trials including 45 029 participants undergoing cognitive assessment, the prevention of nonfatal cardiovascular events in 4.5% of survivors in the Heart Protection Study, by randomization to statin, yielded an estimated cognitive function difference equivalent to avoiding 0.15 years of aging. By contrast, the trial was powered to detect a difference in cognitive aging of at least 1 year.
Abstract
This secondary analysis of 3 randomized clinical trials estimates the effect on cognitive aging of the avoidance of vascular events and evaluates whether reports of nonsignificant results exclude worthwhile benefit among patients with vascular disease.
Abstract
Importance
Acquisition of reliable randomized clinical trial evidence of the effects of cardiovascular interventions on cognitive decline is a priority.
Objectives
To estimate the association of cognitive aging with the avoidance of vascular events in cardiovascular intervention trials and understand whether reports of nonsignificant results exclude worthwhile benefit.
Design, Setting, and Participants
This secondary analysis of 3 randomized clinical trials in participants with preexisting occlusive vascular disease or diabetes included survivors to final in-trial follow-up in the Heart Protection Study (HPS), Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH), and Treatment of HDL (High-Density Lipoprotein) to Reduce the Incidence of Vascular Events (HPS2-THRIVE) trials of lipid modification for prevention of cardiovascular events. Data were collected from February 1994 through January 2013 and analyzed from January 2015 through December 2018.
Main Outcomes and Measures
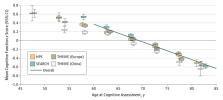
Cognitive function was assessed at the end of a mean (SD) of 4.9 (1.5) years of follow-up using a 14-item verbal test. Associations of the incidence of vascular events and new-onset diabetes during the trials, with cognitive function at final in-trial follow-up were estimated and expressed as years of cognitive aging (using the association of the score with age >60 years). The benefit on cognitive aging mediated through the effects of lowering low-density lipoprotein cholesterol levels on events was estimated by applying these findings to nonfatal event differences observed with statin therapy in the HPS trial.
Results
Among 45 029 participants undergoing cognitive assessment, mean (SD) age was 67.9 (8.0) years; 80.7% were men. Incident stroke (n = 1197) was associated with 7.1 (95% CI, 5.7-8.5) years of cognitive aging; incident transient ischemic attack, myocardial infarction, heart failure, and new-onset diabetes were associated with 1 to 2 years of cognitive aging. In HPS, randomization to statin therapy for 5 years resulted in 2.0% of survivors avoiding a nonfatal stroke or transient ischemic attack and 2.4% avoiding a nonfatal cardiac event, which yielded an expected reduction in cognitive aging of 0.15 (95% CI, 0.11-0.19) years. With 15 926 participants undergoing cognitive assessment, HPS had 80% power to detect a 1-year (ie, 20% during the 5 years) difference in cognitive aging.
Conclusions and Relevance
The expected cognitive benefits of the effects of preventive therapies on cardiovascular events during even the largest randomized clinical trials may have been too small to be detectable. Hence, nonsignificant findings may not provide good evidence of a lack of worthwhile benefit on cognitive function with prolonged use of such therapies.
Trial Registration
isrctn.com and ClinicalTrials.gov Identifiers: ISRCTN48489393, ISRCTN74348595, and NCT00461630
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
A major role for cardiovascular burden in age-related cognitive decline.

- Record: found
- Abstract: found
- Article: found
Cognitive Test Scores in UK Biobank: Data Reduction in 480,416 Participants and Longitudinal Stability in 20,346 Participants
- Record: found
- Abstract: found
- Article: not found