- Record: found
- Abstract: found
- Article: found
Liver Abnormalities in Turner Syndrome: The Importance of Estrogen Replacement
Read this article at
Abstract
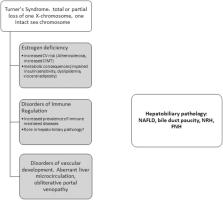
Turner syndrome is one of the most frequently reported sex chromosomal abnormalities, affecting approximately 40 in every 100 000 live female births. The underlying chromosomal alteration is the complete or partial loss of X chromosome or mosaicism. Because of primary ovarian insufficiency, the synthesis of estrogen hormones is compromised, and patients require hormone substitution. Apart from the phenotypical presentation (short stature, primary amenorrhea), the effects of ovarian insufficiency can affect diverse organ systems (such as cardiovascular, endocrine, and lymphatic systems). Hepatobiliary pathology can present on a broad spectrum: from mild asymptomatic hypertransaminasemia to marked architectural changes. Estrogen hormone replacement therapy in these patients can improve the perturbations of laboratory values and can attenuate the progression of hepatic structural changes. Moreover, providing sufficient estrogen replacement has numerous benefits for other conditions of the patients as well. Both the all-cause mortality and deaths from cardiovascular complications are greatly increased in Turner syndrome, and hormone replacement might contribute to the decreased incidence of these events. The diagnostics of Turner syndrome are outside the scope of our paper, and we briefly discuss the cardiovascular complications because many the liver involvement partially involves alterations of vascular origin. Though we sought to highlight the importance of proper hormone replacement therapy, we did not attempt to write a comprehensive recommendation for exact treatment protocols. We provided an overview of preferred therapeutic approaches, as the treatment should be tailored according to the individual patient’s needs.
Related collections
Most cited references74
- Record: found
- Abstract: found
- Article: found
Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US
- Record: found
- Abstract: found
- Article: not found
