- Record: found
- Abstract: found
- Article: found
Subclavian Artery Calcification: A Narrative Review
Read this article at
Abstract
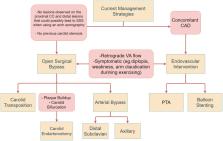
Subclavian artery calcification (SAC) affects 2% of the population and presents a serious risk of developing into subclavian steal syndrome (SSS). Risk factors for plaque formation of the subclavian artery include diabetes, hypertension, and smoking. While SAC generally presents as asymptomatic, symptoms in severe cases may include numbness, pain at rest, and ischemic gangrene. Patients with severe SSS are at high risk of developing neurological symptoms as a result of vertebrobasilar insufficiency affecting posterior cerebral perfusion. On physical examination, SSS is preliminarily diagnosed from bilateral inter-arm systolic blood pressure discrepancy (>10 mmHg), which can be further confirmed with vascular imaging. Duplex ultrasound (DUS) is a cost-effective and non-invasive baseline technique for visualizing luminal stenosis and quantifying peak systolic velocity (PSV). Computed tomography angiography (CTA) provides high-quality, fast, three-dimensional (3D) imaging at the cost of introducing nephrotoxic contrast agents. Magnetic resonance angiography (MRA) is the safest 3D imaging modality, without the use of X-rays and contrast agents, that is useful in assessing plaque characteristics and degree of stenosis. DUS-assisted digital subtraction angiography (DSA) remains the gold standard for grading the degree of stenosis in the subclavian artery and determining the distance between the puncture site and lesion, which can be carried out in a combined procedure with endovascular management strategies. The fundamental treatment options are surgical and endovascular intervention. Endovascular treatment options include percutaneous transluminal angiography (PTA) for recanalization of the stenosed vessel and permanent balloon stenting to prevent collapse after PTA. Overall, the benefits of endovascular management encompass faster recovery, lower stenosis recurrence rate, and lower incidence of complications, making it the treatment of choice in low-risk patients. Surgical interventions, although more complex, are considered gold-standard treatment options.
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
Vascular calcification: an update on mechanisms and challenges in treatment.
- Record: found
- Abstract: found
- Article: not found
Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study.
- Record: found
- Abstract: found
- Article: not found