- Record: found
- Abstract: found
- Article: found
Unmasked immune reconstitution inflammatory syndrome towards B-cell non-Hodgkin lymphoma during treatment of esophageal actinomycosis in a patient with advanced HIV: a case report
Read this article at
Abstract
Background
Actinomycosis is an unusual chronic bacterial infection, even rarer in people living with HIV. It is not considered an AIDS-defining disease. However, the role in co-presentation or overlap with other opportunistic conditions of advanced HIV is unknown.
Case presentation
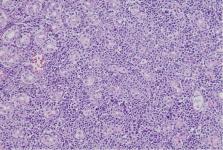
A 49-year-old Peruvian male presented with a 4-month history of dysphagia, odynophagia, hyporexia and wasting. He underwent an upper digestive endoscopy, in which ulcers with a necrotic center were observed, therefore, the initial diagnostic assumption was esophageal cancer. Subsequent pathology report excluded neoplasms and confirmed the diagnosis of actinomycosis. Serology for human immunodeficiency virus was requested, yielding a positive result. Antimicrobial treatment with amoxicillin and antiretroviral therapy were indicated, with slow clinical improvement. After 4 months, epigastric discomfort presented, for which a new upper digestive endoscopy was performed, revealing a deep gastric ulcer, which was compatible with diffuse large B-cell non-Hodgkin lymphoma.
Conclusion
Esophageal actinomycosis in people living with HIV is very rare. We suggest HIV-associated immunosuppression is not enough to allow for actinomycosis to develop, and masked underlying entities should be sought. The existence of such entities in people living with HIV should raise awareness of the possibility of unmasked immune reconstitution inflammatory syndrome once treatment has started.
Related collections
Most cited references17

- Record: found
- Abstract: found
- Article: found
Actinomycosis: etiology, clinical features, diagnosis, treatment, and management
- Record: found
- Abstract: found
- Article: not found
Actinomyces and related organisms in human infections.
- Record: found
- Abstract: found
- Article: not found