- Record: found
- Abstract: found
- Article: found
Inappropriate surgical chemoprophylaxis and surgical site infection rate at a tertiary care teaching hospital
Abstract
Objectives
This study aimed to analyze the pattern of surgical chemoprophylaxis, surgical site infection rate, and to check rationality of surgical chemoprophylaxis based on Kunin's criteria.
Materials and methods
A prospective, observational study was performed on patients undergoing surgery, in a tertiary care teaching hospital. Data were collected in a pro-forma which included the patients’ details, prescriptions from date of admission to discharge or any other outcome and operative notes. Surgical site infection as defined by Centre for Disease Control criteria was recorded. Rationality was assessed based on Kunin's criteria.
Results
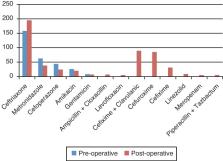
Total 220 patients were enrolled over a period of one year. Mean hospital stay was 8.67 ± 5.17 days. A total of 2294 drugs were prescribed out of which 840 (36.61%) were antimicrobials. Mean duration for pre-operative intravenous antimicrobial therapy was 0.75 ± 0.45 day and for post-operative intravenous antimicrobial therapy was 3.33 ± 2.24 days while post-operative oral antimicrobial therapy was 4.58 ± 3.34 days. Third generation cephalosporins were prescribed most frequently 64.74% and 64.40% pre-operatively and post-operatively respectively. Antimicrobial prescribing was inappropriate in 52.28%. Total of 19 patients developed surgical site infection. Surgical site infection rate was significantly higher (13.04%) in patients receiving inappropriate chemoprophylaxis ( p < 0.01). Surgical site infection adds 9.98 days of hospital stay ( p < 0.0001) and 3.57 extra drugs ( p < 0.0001) compared to group without surgical site infection.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: found
Health and Economic Impact of Surgical Site Infections Diagnosed after Hospital Discharge
- Record: found
- Abstract: found
- Article: not found
Appropriateness of antimicrobial therapy measured by repeated prevalence surveys.
- Record: found
- Abstract: not found
- Article: not found