- Record: found
- Abstract: found
- Article: found
Autonomic symptoms in migraine: Results of a prospective longitudinal study
Read this article at
Abstract
Objective
To assess the prevalence and burden of autonomic symptoms in migraine, and determine the relationship with migraine frequency.
Background
Autonomic symptoms in migraine have been theorized to occur in the setting of inter-ictal sympathetic hypoactivity and hyper-sensitivity. There is limited data prospectively assessing cranial and extra-cranial autonomic symptoms with a validated instrument, or longitudinal data on the relationship between migraine disease activity and autonomic symptoms.
Methods
Patients attending a single tertiary academic center were recruited into a prospective cohort study between September 2020 and June 2022. In addition to standard clinical care, they completed several surveys including the Composite Autonomic Symptom Scale (COMPASS-31) questionnaire, a validated survey of autonomic symptoms.
Results
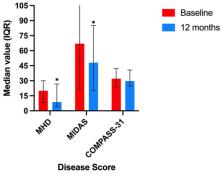
A total of 43 patients (66.7% female, median age 42, IQR 17) were included in the final analysis. There was a baseline 20 monthly headache days (MHD) (IQR 21.7), and 65.1% of the population had chronic migraine by ICHD-3 criteria. A significantly elevated weighted COMPASS-31 score was reported in 60.5% of respondents (mean 30.3, SD 13.3) at baseline. After 12 months treatment, significant improvements were reported in migraine frequency (median MHD 20–8.7) and disability (median Migraine Disability Assessment Score 67–48), but not in autonomic symptoms (mean score 30.3, SD 11.2).
Conclusion
Autonomic symptoms were frequently reported in patients with migraine. However, they did not correlate with headache frequency or reversion to episodic frequency. Further study is required to elucidate specific approaches and treatments for autonomic symptoms, and further evaluate the underlying pathophysiological mechanisms.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
COMPASS 31: a refined and abbreviated Composite Autonomic Symptom Score.
- Record: found
- Abstract: found
- Article: not found
Postural tachycardia syndrome: a heterogeneous and multifactorial disorder.
- Record: found
- Abstract: found
- Article: not found