- Record: found
- Abstract: found
- Article: found
Evaluation of the Benefit of Routine Intraoperative Frozen Section Analysis of Sentinel Lymph Nodes in Breast Cancer
Read this article at
Abstract
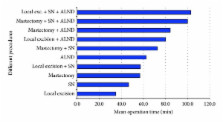
Aims. Intraoperative analysis of the sentinel lymph node (SLN) by frozen section (FS) allows for immediate axillary lymph node dissection (ALND) in case of metastatic disease in patients with breast cancer. The aim of this study is to evaluate the benefit of intraoperative FS, with regard to false negative rate (FNR) and influence on operation time. Materials and Methods. Intraoperative analysis of the SLN by FS was performed on 628 patients between January 2005 and October 2009. Patients were retrospectively studied. Results. FS accurately predicted axillary status in 525 patients (83.6%). There were 78 true positive findings (12.4%), of which there are 66 macrometastases (84.6%), 2 false positive findings (0.3%), and 101 false negative findings (16.1%), of which there are 65 micrometastases and isolated tumour cells (64.4%) resulting in an FNR of 56.4%. Additional operation time of a secondary ALND after wide local excision and SLNB is 17 minutes, in case of ablative surgery 35 minutes. The SLN was negative in 449 patients (71.5%), making their scheduled operation time unnecessary. Conclusions. FS was associated with a high false negative rate (FNR) in our population, and the use of telepathology caused an increase in this rate. Only 12.4% of the patients benefited from intraoperative FS, as secondary ALND could be avoided, so FS may be indicated for a selected group of patients.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial.
- Record: found
- Abstract: found
- Article: not found
Sentinel-lymph-node biopsy as a staging procedure in breast cancer: update of a randomised controlled study.
- Record: found
- Abstract: found
- Article: not found