- Record: found
- Abstract: found
- Article: found
Cancer and stroke: commonly encountered by clinicians, but little evidence to guide clinical approach
Read this article at
Abstract
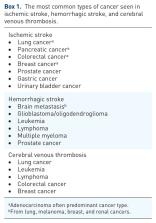
The association between stroke and cancer is well-established. Because of an aging population and longer survival rates, the frequency of synchronous stroke and cancer will become even more common. Different pathophysiologic mechanisms have been proposed how cancer or cancer treatment directly or via coagulation disturbances can mediate stroke. Increased serum levels of D-dimer, fibrin degradation products, and CRP are more often seen in stroke with concomitant cancer, and the clot retrieved during thrombectomy has a more fibrin- and platelet-rich constitution compared with that of atherosclerotic etiology. Multiple infarctions are more common in patients with active cancer compared with those without a cancer diagnosis. New MRI techniques may help in detecting typical patterns seen in the presence of a concomitant cancer. In ischemic stroke patients, a newly published cancer probability score can help clinicians in their decision-making when to suspect an underlying malignancy in a stroke patient and to start cancer-screening studies. Treating stroke patients with synchronous cancer can be a delicate matter. Limited evidence suggests that administration of intravenous thrombolysis appears safe in non-axial intracranial and non-metastatic cancer patients. Endovascular thrombectomy is probably rather safe in these patients, but probably futile in most patients placed on palliative care due to their advanced disease. In this topical review, we discuss the epidemiology, pathophysiology, and prognosis of ischemic and hemorrhagic strokes as well as cerebral venous thrombosis and concomitant cancer. We further summarize the current evidence on acute management and secondary preventive therapy.
Related collections
Most cited references140
- Record: found
- Abstract: found
- Article: not found
Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association
- Record: found
- Abstract: found
- Article: not found
Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials.
- Record: found
- Abstract: found
- Article: not found