- Record: found
- Abstract: found
- Article: found
Gestational weight gain in Chinese women -- results from a retrospective cohort in Changsha, China
Read this article at
Abstract
Background
The generalizability of the gestational weight gain (GWG) ranges recommended by the Institute of Medicine (IOM) to Chinese women is disputed.
Methods
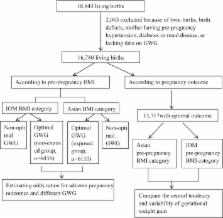
In 2016, 16,780 pregnant women who gave birth to live singletons in Changsha, China, were enrolled. First, subjects with optimal pregnancy outcomes were identified for the GWG percentile distribution description and for comparison to the IOM recommendations. Second, all subjects with optimal GWG according to the IOM body mass index (BMI) cutoffs and those with optimal GWG according to the Asian BMI cutoffs were selected. Pregnancy outcomes were compared between those two groups.
Results
A total of 13,717 births with optimal pregnancy outcomes were selected to describe the GWG distribution. The height and central position of the GWG distributions determined by the Asian BMI cutoffs differed from those determined by the IOM BMI cutoffs among the overweight and obese groups. The recommended IOM GWG ranges were narrower than and shifted to the left of the observed distributions. In both BMI classification schemes, however, the IOM-recommended ranges were within the middle 70% (Pc 15th–85th) and 50% (Pc 25th–75th) of the observed distribution. A total of 6438 (38.37%) and 6110 (36.41%) women gained optimal GWG, according to the IOM and Asian BMI classifications, respectively. Compared with those with optimal GWG according to IOM BMI cutoffs, women with optimal GWG according to the Asian BMI cutoffs had lower risks of both macrosomia (adjusted OR = 0.79, 95%CI: 0.67–0.94) and large-for-gestational age (adjusted OR = 0.86, 95%CI: 0.76, 0.98). However, no significantly different risks of preterm, low birthweight, small-for-gestational age, pregnancy-induced hypertension, or gestational diabetes were found between them.
Related collections
Most cited references21

- Record: found
- Abstract: found
- Article: found
Birth Weight Reference Percentiles for Chinese
- Record: found
- Abstract: found
- Article: not found
The accuracy of self-reported pregnancy-related weight: a systematic review.
- Record: found
- Abstract: found
- Article: not found