- Record: found
- Abstract: found
- Article: found
Insulitis in human type 1 diabetes: lessons from an enigmatic lesion
Read this article at
Abstract
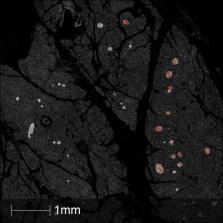
Type 1 diabetes is caused by a deficiency of insulin secretion which has been considered traditionally as the outcome of a precipitous decline in the viability of β-cells in the islets of Langerhans, brought about by autoimmune-mediated attack. Consistent with this, various classes of lymphocyte, as well as cells of the innate immune system have been found in association with islets during disease progression. However, analysis of human pancreas from subjects with type 1 diabetes has revealed that insulitis is often less intense than in equivalent animal models of the disease and can affect many fewer islets than expected, at disease onset. This is especially true in subjects developing type 1 diabetes in, or beyond, their teenage years. Such studies imply that both the phenotype and the number of immune cells present within insulitic lesions can vary among individuals in an age-dependent manner. Additionally, the influent lymphocytes are often mainly arrayed peripherally around islets rather than gaining direct access to the endocrine cell core. Thus, insulitis remains an enigmatic phenomenon in human pancreas and this review seeks to explore the current understanding of its likely role in the progression of type 1 diabetes.
Related collections
Most cited references76
- Record: found
- Abstract: not found
- Article: not found
Pathologic anatomy of the pancreas in juvenile diabetes mellitus.
- Record: found
- Abstract: found
- Article: not found
Precision diabetes: learning from monogenic diabetes
- Record: found
- Abstract: found
- Article: not found