- Record: found
- Abstract: found
- Article: found
Diabetes Fact Sheets in Korea, 2018: An Appraisal of Current Status
Read this article at
Abstract
Background
The objective of this study was to investigate the prevalence, management, and comorbidities of diabetes among Korean adults aged 30 years and older.
Methods
This study used 2013 to 2016 data from the Korea National Health and Nutrition Examination Survey, a nationally-representative survey of the Korean population. Diabetes was defined as fasting glucose ≥126 mg/dL, current use of antidiabetic medication, a previous history of diabetes, or glycosylated hemoglobin (HbA1c) ≥6.5%.
Results
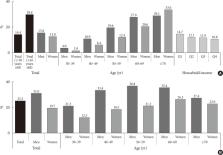
In 2016, 14.4% (approximately 5.02 million) of Korean adults had diabetes. The prevalence of impaired fasting glucose was 25.3% (8.71 million). From 2013 to 2016, the awareness, control, and treatment rates for diabetes were 62.6%, 56.7%, and 25.1%, respectively. People with diabetes had the following comorbidities: obesity (50.4%), abdominal obesity (47.8%), hypertension (55.3%), and hypercholesterolemia (34.9%). The 25.1%, 68.4%, and 44.2% of people with diabetes achieved HbA1c <6.5%, blood pressure <140/85 mm Hg, and low density lipoprotein cholesterol <100 mg/dL. Only 8.4% of people with diabetes had good control of all three targets.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001.
- Record: found
- Abstract: found
- Article: not found
Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes.
- Record: found
- Abstract: found
- Article: not found