- Record: found
- Abstract: found
- Article: found
Influences on patient satisfaction in healthcare centers: a semi-quantitative study over 5 years
Read this article at
Abstract
Background
Knowledge of ambulatory patients’ satisfaction with clinic visits help improve communication and delivery of healthcare. The goal was to examine patient satisfaction in a primary care setting, identify how selected patient and physician setting and characteristics affected satisfaction, and determine if feedback provided to medical directors over time impacted patient satisfaction.
Methods
A three-phase, semi-quantitative analysis was performed using anonymous, validated patient satisfaction surveys collected from 889 ambulatory outpatients in 6 healthcare centers over 5-years. Patients’ responses to 21 questions were analyzed by principal components varimax rotated factor analysis. Three classifiable components emerged: Satisfaction with Physician, Availability/Convenience, and Orderly/Time. To study the effects of several independent variables (location of clinics, patients’ and physicians’ age, education level and duration at the clinic), data were subjected to multivariate analysis of variance (MANOVA)..
Results
Changes in the healthcare centers over time were not significantly related to patient satisfaction. However, location of the center did affect satisfaction. Urban patients were more satisfied with their physicians than rural, and inner city patients were less satisfied than urban or rural on Availability/Convenience and less satisfied than urban patients on Orderly/Time.
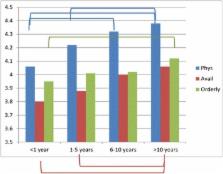
How long a patient attended a center most affected satisfaction, with patients attending >10 years more satisfied in all three components than those attending <1–5 years. Level of education affected patients’ satisfaction only in the component Orderly/Time; patients without a high school education were significantly less satisfied than those with more. Patients in their 40′s were significantly less satisfied in Availability/Convenience than those >60 years old.
Patients were significantly more satisfied with their 30–40 year-old physicians compared with those over 60. On Orderly/Time, patients were more satisfied with physicians who were in their 50′s than physicians >60.
Conclusions
Improvement in patient satisfaction includes a need for immediate, specific feedback. Although Medical Directors received feedback yearly, we found no significant changes in patient satisfaction over time. Our results suggest that, to increase satisfaction, patients with lower education, those who are sicker, and those who are new to the center likely would benefit from additional high quality interactions with their physicians.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity.
- Record: found
- Abstract: found
- Article: not found
Patient-physician social concordance, medical visit communication and patients' perceptions of health care quality.
- Record: found
- Abstract: found
- Article: not found