- Record: found
- Abstract: found
- Article: found
Short-term treatment of irbesartan and hydrochlorothiazide decreases plasma N-terminal pro-brain natriuretic peptide levels in subjects with acute exacerbations of COPD
Abstract
Background
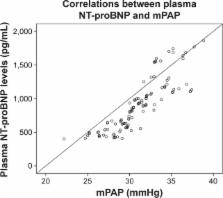
Plasma levels of N-terminal pro-brain natriuretic peptide (NT-proBNP) are elevated in subjects with COPD, and high plasma NT-proBNP levels are correlated with a poor prognosis. Thus, it is crucial to decrease the plasma NT-proBNP levels at the early stage of disease. We aimed to assess the effects of short-term treatment of irbesartan and hydrochlorothiazide on plasma NT-proBNP levels and health-related quality of life (HRQOL) in subjects with acute exacerbations of COPD (AECOPD).
Subjects and methods
Eighty subjects with AECOPD and high plasma NT-proBNP levels, without any clinical evidence of cor pulmonale, were enrolled. The subjects were randomly allocated into two groups of 40 subjects. In addition to standard treatment for AECOPD, the subjects in group I were treated with irbesartan alone, and those in group II were treated with irbesartan and hydrochlorothiazide for a week. Forty subjects with stable COPD were enrolled as a control group. Plasma NT-proBNP concentrations were measured on admission and on the first, fourth, and seventh days. The subjects’ health-related quality of life was evaluated applying the 36-item short-form questionnaire on the first day before treatment and on the seventh day after treatment.
Results
Treatment of irbesartan and hydrochlorothiazide significantly decreased plasma NT-proBNP levels in subjects with AECOPD, and this reduction was more significant in group II than that in group I. There were no significant differences in 36-item short-form domain scores between subjects with stable COPD and those with AECOPD who were treated with irbesartan and hydrochlorothiazide.
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure.
- Record: found
- Abstract: found
- Article: not found
Prognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressure.
- Record: found
- Abstract: found
- Article: not found