- Record: found
- Abstract: found
- Article: found
A 7-Year Brazilian National Perspective on Plasmid-Mediated Carbapenem Resistance in Enterobacterales, Pseudomonas aeruginosa, and Acinetobacter baumannii Complex and the Impact of the Coronavirus Disease 2019 Pandemic on Their Occurrence
Read this article at
Abstract
Background
Carbapenemase production is a global public health threat. Antimicrobial resistance (AMR) data analysis is critical to public health policy. Here we analyzed carbapenemase detection trends using the AMR Brazilian Surveillance Network.
Methods
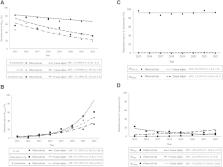
Carbapenemase detection data from Brazilian hospitals included in the public laboratory information system dataset were evaluated. The detection rate (DR) was defined as carbapenemase detected by gene tested per isolate per year. The temporal trends were estimated using the Prais–Winsten regression model. The impact of COVID-19 on carbapenemase genes in Brazil was determined for the period 2015–2022. Detection pre- (October 2017 to March 2020) and post-pandemic onset (April 2020 to September 2022) was compared using the χ 2 test. Analyses were performed with Stata 17.0 (StataCorp, College Station, TX).
Results
83 282 bla KPC and 86 038 bla NDM were tested for all microorganisms. Enterobacterales DR for bla KPC and bla NDM was 68.6% (41 301/60 205) and 14.4% (8377/58 172), respectively. P. aeruginosa DR for bla NDM was 2.5% (313/12 528). An annual percent increase for bla NDM of 41.1% was observed, and a decrease for bla KPC of −4.0% in Enterobacterales, and an annual increase for bla NDM of 71.6% and for bla KPC of 22.2% in P. aeruginosa. From 2020 to 2022, overall increases of 65.2% for Enterobacterales, 77.7% for ABC, and 61.3% for P. aeruginosa were observed in the total isolates.
Abstract
Seven-year surveillance in Brazil showed a >60% increase in resistance genes during the COVID-19 pandemic, especially bla NDM in Enterobacterales and Pseudomonas aeruginosa. bla KPC in Enterobacterales and bla SPM in P. aeruginosa decreased. These data contribute to Antimicrobial Resistance public policies.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study
- Record: found
- Abstract: found
- Article: not found
Bacterial and fungal co-infection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing
- Record: found
- Abstract: found
- Article: not found