- Record: found
- Abstract: found
- Article: found
Balloon-occluded retrograde transvenous obliteration for gastric varices: the relationship between the clinical outcome and gastrorenal shunt occlusion
Read this article at
Abstract
Background
The rupture of gastric varices is associated with high mortality rate. Balloon-occluded retrograde transvenous obliteration (B-RTO), a minimally invasive procedure that was introduced in the mid-1990s, has been widely accepted in Japan. Several reports have indicated that B-RTO yields satisfactory results; however, few reports have discussed the recurrence of gastric varices after this therapy. The purpose of this study is to retrospectively evaluate the technical aspects of B-RTO and the recurrence of gastric varices after treatment with this procedure.
Methods
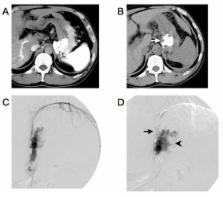
B-RTO was performed in 47 patients with gastric varices, who were at a risk of variceal ruptures and who may or may not have had a history of variceal bleeding. We injected a sclerosing agent into the gastric varices for 30-60 minutes. To evaluate the therapeutic efficacy of the technique, we obtained contrast-enhanced computed tomography (CT) scans 5 days after B-RTO. As a general rule, if the gastric varices did not appear thrombosed, we repeated the procedure 7 days after the first procedure.
Results
B-RTO was a technical success in 37 patients. It was performed once in 26 patients, twice in 6 patients, thrice in 2 patients, and 4 times in 3 patients. Contrast-enhanced CT scans obtained after B-RTO showed thrombosed gastrorenal shunts in 29 patients and patent gastrorenal shunts in 8 patients. The gastric varices recurred in 2 patients who had patent gastrorenal shunts. The overall cumulative relapse-free rate of gastric varices was 90% at 5 years after B-RTO.
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients.
- Record: found
- Abstract: found
- Article: not found
Retrograde transvenous obliteration of gastric varices.
- Record: found
- Abstract: found
- Article: not found