- Record: found
- Abstract: found
- Article: found
Association between Chinese visceral adiposity index and metabolic-associated fatty liver disease in Chinese adults with type 2 diabetes mellitus
Read this article at
Abstract
Objective
The purpose of the study was to determine the correlation of the Chinese visceral adiposity index (CVAI) with metabolic-associated fatty liver disease (MAFLD) in Chinese adults with type 2 diabetes mellitus (T2DM).
Materials/methods
In this cross-sectional study, data on sociodemographic characteristics, laboratory test results, coexisting diseases, and medical therapy were collected and analyzed. Multivariate logistic regression analyses were used to examine the correlation between CVAI and MAFLD. In order to investigate the correlation between CVAI on a continuous scale and MAFLD, a restricted cubic spline (RCS) was used.
Results
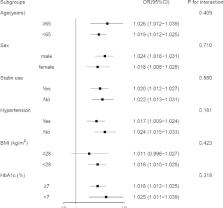
A total of 679 participants were included in this study. There were 251 female participants and 428 male participants, with a median age of 55 years. In the multivariate logistic regression model, diastolic blood pressure, duration of diabetes, glycated hemoglobin, hemoglobin, alanine transaminase, aspartate aminotransferase, gamma -glutamyl transferase, albumin, blood urea nitrogen, total cholesterol, low-density lipoprotein cholesterol, statin use and metformin use were adjusted, and an evident increase in the odds ratios of MAFLD from the lowest to the highest CVAI quartile was found ( P value for trend < 0.001). Moreover, the RCS curves revealed a positive correlation between CVAI and MAFLD.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
WITHDRAWN: Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition
- Record: found
- Abstract: found
- Article: not found
A new definition for metabolic associated fatty liver disease: an international expert consensus statement
- Record: found
- Abstract: found
- Article: not found