- Record: found
- Abstract: found
- Article: found
Utility of the REBA MTB-rifa® assay for rapid detection of rifampicin resistant Mycobacterium Tuberculosis
Read this article at
Abstract
Background
Drug-resistant tuberculosis (TB), including resistance to both rifampicin (RIF) and isoniazid (INH) referred to as multidrug-resistant tuberculosis (MDR-TB), has become an increasing global threat in recent years. Effective management of patients infected with MDR-TB strains requires identifying such patients by performing conventional drug-susceptibility testing (DST) on bacteria isolated from sputum, a process that can take up to 2 months. This delay in diagnosis can result in worsening and continued transmission of MDR-TB. Molecular methods that rely upon nucleic acid amplification of specific alleles known to be associated with resistance to specific drugs have been helpful in shortening the time to detect drug resistant TB.
Methods
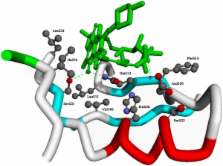
We investigated the utility of the REBA MTB-Rifa®, a commercially available line probe assay (LPA) for detecting rifampicin (RIF) resistance in the RIF resistance-determining region (RRDR) of the rpoB gene. Altogether, 492 Mycobacterium tuberculosis ( M. tuberculosis) clinical isolates and additional 228 smear- and culture-positive sputum samples with confirmed M. tuberculosis were collected from subjects with suspected MDR-TB in South Korea. The results were compared with conventional phenotypic DST and sequencing of the rpoB gene.
Results
A total of 215 of the 492 isolates were resistant to RIF by conventional DST, and of which 92.1% (198/215) were MDR-TB strains. The REBA MTB-Rifa® assay identified RIF resistance in 98.1% (211/215) of these isolates but failed to identify resistance in four phenotypically RIF resistant isolates. These four isolates lacked mutations in the RRDR but three were confirmed to be MDR-TB strains by sequencing. The sensitivity and specificity of this test for clinical isolates was thus 98.1% (211/215) and 100% (277/277), respectively. When applied directly to 228 smear positive sputum samples, the sensitivity and the specificity of REBA MTB-Rifa® assay was 100% (96/96, 132/132), respectively.
Conclusions
These findings support the use of the REBA MTB-Rifa® assay for rapid detection of RIF resistance on clinical isolates and smear positive sputum samples. The results also suggest that RIF resistance is a good surrogate marker of MDR-TB in South Korea and the need to add more probes to other LPAs which can cover newly identified mutations relevant to RIF resistance.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update.
- Record: found
- Abstract: found
- Article: not found
Rapid, low-technology MIC determination with clinical Mycobacterium tuberculosis isolates by using the microplate Alamar Blue assay.

- Record: found
- Abstract: found
- Article: found