- Record: found
- Abstract: found
- Article: found
Interval from Prostate Biopsy to Radical Prostatectomy Does Not Affect Immediate Operative Outcomes for Open or Minimally Invasive Approach

Read this article at
Abstract
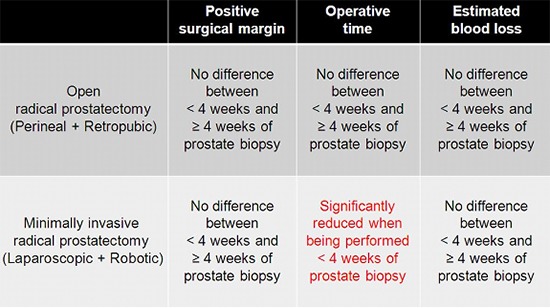
Traditionally, urologists recommend an interval of at least 4 weeks after prostate biopsy before radical prostatectomy. The aim of our study was to evaluate whether the interval from prostate biopsy to radical prostatectomy affects immediate operative outcomes, with a focus on differences in surgical approach. The study population of 1,848 radical prostatectomy patients was divided into two groups according to the surgical approach: open or minimally invasive. Open group included perineal and retropubic approach, and minimally invasive group included laparoscopic and robotic approach. The cut-off of the biopsy-to-surgery interval was 4 weeks. Positive surgical margin status, operative time and estimated blood loss were evaluated as endpoint parameters. In the open group, there were significant differences in operative time and estimated blood loss between the <4-week and ≥4-week interval subgroups, but there was no difference in positive margin rate. In the minimally invasive group, there were no differences in the three outcome parameters between the two subgroups. Multivariate analysis revealed that the biopsy-to-surgery interval was not a significant factor affecting immediate operative outcomes in both open and minimally invasive groups, with the exception of the interval ≥4 weeks as a significant factor decreasing operative time in the minimally invasive group. In conclusion, performing open or minimally invasive radical prostatectomy within 4 weeks of prostate biopsy is feasible for both approaches, and is even beneficial for minimally invasive radical prostatectomy to reduce operative time.
Related collections
Most cited references23
- Record: found
- Abstract: not found
- Article: not found
The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma.
- Record: found
- Abstract: found
- Article: not found
Pathophysiology of acute wound healing.
- Record: found
- Abstract: found
- Article: not found