- Record: found
- Abstract: found
- Article: found
The Value of IGF-1 and IGFBP-1 in Patients With Heart Failure With Reduced, Mid-range, and Preserved Ejection Fraction
Read this article at
Abstract
Background
Previous studies have reported inconsistent results regarding the implications of deranged insulin-like growth factor 1 (IGF-1)/insulin-like growth factor-binding protein 1 (IGFBP-1) axis in patients with heart failure (HF). This study evaluates the roles of IGF1/IGFBP-1 axis in patients with HF with reduced ejection fraction (HFrEF), mid-range ejection fraction (HFmrEF), or preserved ejection fraction (HFpEF).
Methods
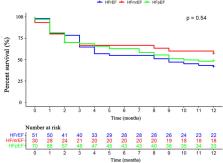
Consecutive patients with HFrEF, HFmrEF, and HFpEF who underwent comprehensive cardiac assessment were included. The primary endpoint was the composite endpoint of all-cause death and HF rehospitalization at one year.
Results
A total of 151 patients with HF (HFrEF: n = 51; HFmrEF: n = 30; HFpEF: n = 70) and 50 control subjects were included. The concentrations of IGFBP-1 ( p < 0.001) and IGFBP-1/IGF-1 ratio ( p < 0.001) were significantly lower in patients with HF compared to controls and can readily distinguish patients with and without HF (IGFBP-1: areas under the curve (AUC): 0.725, p < 0.001; IGFBP-1/IGF-1 ratio: AUC:0.755, p < 0.001; respectively). The concentrations of IGF-1, IGFBP-1, and IGFBP-1/IGF-1 ratio were similar among HFpEF, HFmrEF, and HFrEF patients. IGFBP-1 and IGFBP-1/IGF-1 ratio positively correlated with N-terminal probrain natriuretic peptide (NT-proBNP) levels ( r = 0.255, p = 0.002; r = 0.224, p = 0.007, respectively). IGF-1, IGFBP-1, and IGFBP-1/IGF-1 ratio did not predict the primary endpoint at 1 year for the whole patients with HF and HF subtypes on both univariable and multivariable Cox regression.
Related collections
Most cited references42
- Record: found
- Abstract: not found
- Article: not found
2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC.
- Record: found
- Abstract: found
- Article: not found
Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group.
- Record: found
- Abstract: found
- Article: not found